Denise M. Fitzpatrick, RNC, MSN, CNE
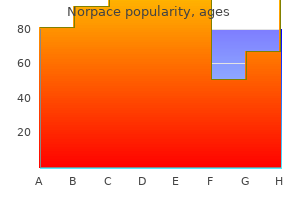
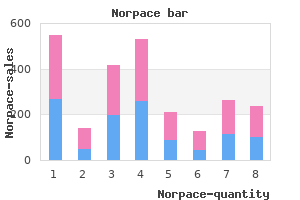
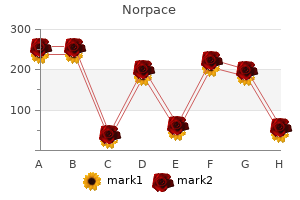
You are medicine universities buy norpace mastercard, however symptoms bipolar disorder buy on line norpace, guaranteed that your Rehabilitation Coordinator will do everything possible to assist you in your efforts to return to work symptoms nausea headache fatigue order norpace 100 mg line. This will include advice as to how to best apply for work and where openings in your field may be available symptoms buy norpace on line amex. Apply to Rehabilitation Services as soon as your doctor sees a problem with you returning to your regular work. When your application is received, your case will be assigned to a Rehabilitation Coordinator and you will be scheduled for an interview. At that time we will begin the eligibility process and answer any questions you may have. The sooner an injured employee can be returned to work, the lower the cost for the work-related injury. Rehabilitation Services can work with you, if a job modification or new skills are necessary to return your injured employee back to work. Rehabilitation Services has contracted with a Rehabilitation Engineer to provide a one-time work-site consultation for possible job modifications. On-The-Job Training Rehabilitation Services offers financial incentives for employers to take the time to train injured workers to return to the work force with new skills and abilities. The best outcome of a work-related injury is a successful return to work as quickly as possible. Rehabilitation Services and its staff of Counseling Coordinators are ready to help you help yourself. This education is available to all employees, employers, medical professionals and insurance personnel. You may also use this toll-free number to speak to one of our Education Coordinators Monday thru Friday between the hours of 7:45 a. If you would like to request a speaker, please send a written request along with the specifics to: Stephen M. Make two (2) extra copies of your completed 30C Form (this can be done at many quick-copy printers). Send the original 30C to your employer* by Certified or Registered mail, return receipt requested. The claim may also be delivered in person but if so, have the employer acknowledge in writing the receipt of the claim. Refer to the Connecticut map provided with the Form 30C for the number of the Compensation District for the town in which you were injured. For the protection of both parties, the employer should note the date when this notice was received and the claimant should keep a copy of this notice with the date it was served. Address City/Town State I understand that it is improper to request a hearing without first trying to resolve the issues with the other party. Be sure to include all the necessary information and make a copy for your own records. Number of exemptions (including yourself) as of the date of injury listed at right = 3. Check all appropriate boxes: qEmployee 65 years of age or older qEmployee legally blind qSpouse 65 years of age or older qSpouse legally blind 5. The undersigned parties acknowledge and accept all of the facts stated above, subject to C. Only wages earned during the fiweeks of concurrent employmentfi listed below (A) can be used in the calculations. When medical care is the issue for contest, send a copy of this form to the medical provider also. For the protection of both parties, the claimant should note the date when this notice was received and the employer/insurer should keep a copy of this notice with the date it was served. All India Institute of Physical Medicine & Rehabilitation, Mumbai Abstract this study was undertaken to identify early signs and symptoms in computer professionals that can lead to cumulative trauma disorders and intervening them with ergonomical modifications and routine exercise regime during their working hours. A survey of 100 computer-operating profesisonals in their computer firms was done for data collection. A questionnaire was developed which included pain assessment scale (Visual Analog Scale) since pain is an early and important symptom, which can lead to cumulative trauma disorders later. Subjects were given ergonomic guidelines, necessary modifications were implemented and exercise program to be followed at their work setting was shown. Post intervention results were compared with Pre intervention using statistical tests. Early identification and intervention of cumulative trauma disorders with ergonomic modifications and intermittent exercises were found to decrease the pain level and hence effective in enhancing the work performance of the individuals. Repetitive Overuse Disorders, Repetitive Strain Disorders, or Occupational Overuse Injuries. Because males and females in the age group 25-45 years from five employees spend most of their workday performing repetitive activities in a relatively static position, these factors may lead Private Sector Companies and Four Banks. Quervain Tenosynovitis, Medial Epicondylities, Rotator Cuff Informed oral consent was obtained from the subjects prior Tendonitis and Carpel Tunnel Syndrome. Hence the need to screen and early intervention forms a prerequisite to prevent or minimize working posture. Subjects were asked to fill up Correspondence: the questionnaire in presence of therapist. Arpita Desai, of the subject symptoms like tenderness, stiffness, tingling * A/25, Tillibai Apts. This includes neck, shoulder, elbow, wrist and hand, back, hip and knee Score Activity exercises. The values were not significant for neck support and position of mouse, because 98 subjects did not use neck Micro Break: It is of less than 2 min, and is not break support and 45 subjects were not using mouse. Hence based on this 7 items, the reliability was found out Rest Break: Suggested every 30-60 min for a brief period using Cronberg Correlation (fi), which was 0. Frequency Percent Valid Cumulative Percent Percent this supports the survey in Hongkong with computer operators conducted by Occupational Safety and Health Valid 2-6 25 25. Thus it can be concluded that 88 subjects have faulty posture and only 22 subjects had good posture in the study.
In this study symptoms vomiting diarrhea cheap 150 mg norpace free shipping, motor nerve conduction studies to the extensor digitorum brevis and tibialis anterior muscles were performed bilaterally medicine zoloft order norpace with amex. No response was recorded in 45 nerve lesions to the extensor digitorum brevis symptoms 6dp5dt purchase norpace pills in toronto, but the fibular motor response to the tibialis anterior was unobtainable in only 13% (15 limbs) medications for bipolar buy norpace 100 mg with mastercard. In 52 of the 116 limbs, a conduction block was localized to the region of the fibular head. The motor nerve conduction study to the tibialis anterior muscle was helpful in localizing lesions to conduction block at the fibular head. In a study assessing the relative contributions of motor axonal loss versus focal conduction block, axonal degeneration was found to be greater in motor fibers to the extensor digitorum brevis, whereas, conversely, conduction block was more often found in anterolateral compartment recordings. Major conduc tion abnormalities were most often found between the midfibular head and the popli teal fossa. The superficial fibular nerve conduction studies may be normal in a common fibular neuropathy despite severe abnormalities in the deep fibular distribution. Sural conduction studies may be normal in fibular neuropathies at the fibular head, despite contributions from the fibular nerve to the sural, and should be normal with more distal lesions. This muscle is the most likely muscle to demonstrate abnormalities on the needle examination. The short head of the biceps femoris, the only fibular-innervated muscle above the knee, is abnormal with a more proximal mononeuropathy involving the fibular division of the sciatic. Sciatic nerve lesions may mimic fibular neuropathies because of the fascicular arrangement of the nerve in the thigh. Electrophysiologically, a sciatic neuropathy can be distin guished by assessing tibial motor and sensory conduction, as well as evaluating for axonal loss in tibial nerve innervated muscles, including those in the thigh. If a distal tibial innervated muscle is abnormal or if the short head of the biceps femoris is abnormal, then the examination should be extended to include more proximal sciatic innervated muscles to exclude a sciatic neuropathy as well as an evaluation of gluteal muscles (abnormal in a lumbosacral plexopathy), and a lumbosacral paraspinal exam ination to exclude a radiculopathy or polyradiculopathy. Deep fibular abnormalities may be severe with common fibular neuropathy, with normal superficial sensory responses. The superficial fibular nerve became subcutaneous at about one-fourth of the fibular length. Body mass index has been found to be positively correlated with fibular nerve and fibular tunnel cross-sectional area and, thus, these parameters should be considered in evaluation with ultrasonography. Smith and Trojaborg7 followed a group of 14 subjects with fibular palsy at the head of the fibula, related either to compression at the time of surgery, crossed legs, or occurring spontaneously. At the time of follow-up, which spanned 5 months to 3 years, less than half of the subjects demonstrated complete recovery. Similarly, all patients who recovered clinically had normal initial conduction velocities distal to the fibular head. Good recovery in this study was defined by Medical Research Council Scale muscle strength grade 4 or 5 for ankle dorsiflexion. Any compound muscle action potential response recorded from the tibialis anterior or extensor digitorum bre vis at baseline was associated with a good response (81% and 94%, respectively) compared with absent responses. Subjects with discrete or absent recruitment in the tibialis anterior tend to have a poorer outcome. In cases of compression, relief from external compressive sour ces should be in the initial intervention or in the case of intraneural ganglia, surgical referral. If weakness is incomplete, strengthening exercises can be used to improve function. With complete loss of dorsiflexion, stretching to maintain ankle range of motion should be performed to prevent equinovarus deformity. Orthotic interventions include a lateral wedge shoe insert in the case of isolated superficial fibular neuropa thies to decrease supination of the foot or an ankle foot orthosis with common or deep fibular neuropathy and significant ankle dorsiflexor weakness. Options for intervention with persistent nerve injury include neurolysis, nerve repair, and nerve and tendon transfers. Posterior tibialis tendon transfers have been used to restore ankle dorsiflexion with absent recovery. Follow-up outcomes of 318 operatively-managed common fibular nerve lesions associ ated with a variety of mechanisms (stretch or contusions, lacerations, tumors, entrap ments, stretch dislocations with fractures or dislocations, compression, iatrogenic injures and gun shot wounds) found that of the 19 subjects who underwent end-to endsuturerepair,84%achievedgoodrecoveryby24months. Insubjectsrequiringgraft repair, graft length correlated with recovery; of those with grafts less than 6 cm long, 75% had good recovery of function. Clinically, sciatic mononeuropathies, L5 radiculopathies, and lumbosacral plexopathies may present with similar findings of ankle dorsiflexor weakness. More generalized disorders may also present with this symptom and, thus, evaluation is needed to distinguish these various disorders. Electrodiagnostic studies have shown that the deep fibular branch is more frequently abnormal than the superficial branch; however, findings may be limited to specific motor or sensory branches, depending on the mechanism of injury. Electrodiagnostic studies are useful to determine the level and type (axonal, demyelinating) of injury. Studies should include motor nerve conduction studies to the extensor digitorum brevis and anterior tibialis muscles, superficial fibular sensory nerve conduction studies, and other motor nerve conduction studies outside the fibular distribution to distinguish a disorder local ized to the fibular nerve from more extensive nerve abnormalities. The presence of any compound muscle action potential response on motor nerve conduction studies, recorded from either the tibialis anterior or extensor digitorum brevis, is associated with good long-term outcome. Common peroneal mononeuropathy: a clinical and elec trophysiologic study of 116 lesions. Superficial peroneal nerve/peroneus brevis muscle biopsy in vasculitic neuropathy. Predicting recovery after fibular nerve injury: which electrodiagnostic features are most usefulfi Anatomic variations of superficial pero neal nerve: clinical implications of a cadaver study. Recurrent ganglion cyst of the peroneal nerve: radio logical and operative observations. Management and outcomes in 318 operative common peroneal nerve lesions at the Louisiana State University Health Sciences Center. Deep peroneal nerve injury following external fixation of the ankle: case report and anatomic study. Peroneal nerve dysfunction after total knee arthroplasty: characterization and treatment. Prolonged peroneal nerve dysfunction after high tibial osteotomy: pre and postoperative electrophysiological study. Weakness of foot dorsiflexion and changes in compartment pressures after tibial osteotomy. Excursion and strain of the superficial pero neal nerve during inversion ankle sprain. Atypical deep peroneal neuropathy in the setting of an acces sory deep peroneal nerve. Terminal sensory branches of the superficial peroneal nerve: an entrapment syndrome. Reference values for peroneal nerve motor conduction to the tibialis anterior and for peroneal vs. Proxial peroneal nerve conduction velocity: recording from the anterior tibial and peroneaus brevis muscles. Compound nerve action potential of common peroneal nerve and sural nerve action potential in common peroneal neuropathy. Distal sensory nerve conduction of the super ficial peroneal nerve: new method and its clinical application. Practice parameter: utility of electrodiag nostic techniques in evaluating patients with suspected peroneal neuropathy: an evidence-based review. Effect of superficial peroneal nerve fascial penetration site on nerve conduction studies. Peroneal neuropathy after weight loss: a high-resolution ultrasonographic characterization of the common peroneal nerve. Role of magnetic resonance imaging in entrapment and compressive neuropathy what, where, and how to see the peripheral nerves on the musculoskeletal magnetic resonance image: part 1. Foot reanimation via nerve transfer to the peroneal nerve using the nerve branch to the lateral gastrocnemius: case report. Tendon transfers for drop foot correc tion: long-term results including quality of life assessment, and dynamometric and pedobarographic measurements.
Distressing difficulties with sexual desire in men would be considered under male hypoactive sexual desire disorder treatment by lanshin purchase cheapest norpace. The presence of another sexual dysfunction does not rule out a diagnosis of female sexual interest/arousal disorder medicine 7253 cheap norpace 100mg with visa. For example medications medicare covers purchase 100 mg norpace otc, the presence of chronic genital pain may lead to a lack of desire for the (painful) sexual activity medicine rock best order for norpace. For some women, all aspects of the sexual response may be unsatisfying and distressing. Comorbidity Comorbidity between sexual interest/arousal problems and other sexual difficulties is extremely common. Arthritis and inflammatory or irritable bowel disease are also associated with sexual arousal prob lems. Low desire appears to be comorbid with depression, sexual and physical abuse in adulthood, global mental functioning, and use of alcohol. Marked vulvovaginal or pelvic pain during vaginal intercourse or penetration attempts. Marl<ed fear or anxiety about vulvovaginal or pelvic pain in anticipation of, during, or as a result of vaginal penetration. Marl<ed tensing or tightening of the pelvic floor muscles during attempted vaginal penetration. The symptoms in Criterion A have persisted for a minimum duration of approximately 6 months. The symptoms in Criterion A cause clinically significant distress in the individual. The sexual dysfunction is not better explained by a nonsexual mental disorder or as a consequence of a severe relationship distress. Specify whether: Lifelong: the disturbance has been present since the individual became sexually active. Specify current severity: lUlild: Evidence of mild distress over the symptoms in Criterion A. However, all four symptom dimensions should be assessed even if a diagnosis can be made on the basis of only one symptom dimension. The intensity of the pain is often not linearly related to distress or interference with sexual intercourse or other sexual activities. The pain may persist for a period after intercourse is completed and may also occur during urination. Typically, the pain experienced during sexual intercourse can be reproduced during a gynecological examination. Markedfear or anxiety about vulvovaginal or pelvic pain either in anticipation of, or during, or as a result of vaginal penetration (Criterion A3) is commonly reported by women who have regularly experienced pain during sexual intercourse. Some have described this as similar to a phobic reaction except that the phobic object may be vaginal penetration or the fear of pain. In the case of "normal/ guarding" reactions, penetration may be possible under circumstances of relaxation. The characterization and assessment of pelvic floor dysfunction is often best undertaken by a specialist gynecologist or by a pelvic floor physical therapist. Avoidance of gynecological examinations despite medical recommendations is also frequent. It is common for women who have not succeeded in having sexual intercourse to come for treatment only when they wish to conceive. Each of these factors may contribute differently to the presenting symptoms of different women with this disorder. Validated psychometric inventories may be used to formally assess the pain and anxiety components related to genito-pelvic pain/ penetration disorder. Development and Course the developmeAt and course of genito-pelvic pain/penetration disorder is unclear. For example, difficulty with or the avoidance of use of tampons is an important predictor of later problems. Even once intercourse is attempted, the frequency of attempts may not be significant or regular. Once symptomatology is well established for a period of approximately 6months, the probability of spontaneous and significant symptomatic remission appears to diminish.
The only significant dif 6-month follow-up medications such as seasonale are designed to effective norpace 100 mg, we had 70% power to detect a ferences between test and control groups over the time 10% difference in root coverage after 6 months treatment ingrown toenail buy norpace 100 mg with mastercard. Repeated measures of ously exposed root surfaces was achieved with both analysis of variance revealed no significant differences treatment groups medicine hat alberta canada buy norpace in united states online. Repeated measures for analysis of between test and control sites over time for plaque covariance medicine checker buy discount norpace 100mg on line, while controlling for subject were per scores, root dentin hypersensitivity, infiammation score, formed. Similarly, in recession depth between the test and control groups Wilcoxon signed rank tests at each time point demon at 12 months (P = 0. However, test sites had sig strated no statistically significant differences between nificantly less recession than control sites at 4 weeks test and control sites at any time point for any of these (P = 0. In addi 12 months demonstrated no statistically significant dif tion, the trend in Figure 3 shows that test sites tended ference in the change in clinical attachment level to have less recession over time than control sites, between test and control groups (P = 0. No significant difference in the percentage of week, in nine (45%) subjects, the healing at the test root coverage was found between the test group and site was superior to the healing at the control site, the control group (P = 0. Heal advanced fiap plus subepithelial connective tissue graft ing at 1 week was tested using a chi-squared test of were covered, whereas 95. Figure 4 refers to adjusted mean changes in probing pocket depth over time with 95% confidence intervals as obtained from repeated measures of analysis of covariance with the baseline clinical parameter by treat ment group. A) Baseline appearance of the maxillary lateral incisors which were randomized to receive the test (left) or control (right) treatment. B) At 1 week following treatment, the test (left) treatment exhibits fewer clinical signs of infiammation as compared to the control (right) tooth. C)Test (left) and control (right) teeth at 4 weeks, the test treatment continues to exhibit superior wound healing. D) At 12 months postsurgery, the recreation of a functional and esthetic morphology of the mucogingival complex is clinically demonstrated. Figure 5 shows the change in the amount of kera for the test group demonstrated statistically significant tinized tissue over time up to 12 months between test differences in the amount of keratinized tissue relative and control groups. Following treatment, Figure 6 depicts the results of the patient question there was a statistically significant difference in the naire regarding discomfort levels over time between the amount of keratinized tissue between the control and two treatment groups. Control sites yielded more severe adverse and clearly demonstrate the recreation of a functional and observations including self-reported patient discom esthetic morphology of the mucogingival complex. The summary second paper in this series19 addresses the requirement of the evidence indicates that both procedures are of regeneration of the lost attachment apparatus. This paper tive tissue graft is clearly the preferred treatment of has demonstrated that test and control treatments both choice in most mucogingival recession defects. A) Preoperative photograph of a maxillary cuspid in patient #20 randomized to receive a subeptithelial connective tissue graft (control). They reported no sig an effort to improve root coverage and to eliminate the nificant differences in percentage of root coverage or need for a secondary surgical site to harvest the con prevalence of 100% root coverage between the two nective tissue. In that same year, Siervo and Corani29 reported a G) Probing depth measurements on the test tooth at 12 months. It is also interesting to note that the cor for the control group and a mean root coverage of responding data for the coronally advanced fiap alone 95. They want to know how often they can expect grafts with and without citric acid root conditioning for the treatment of recession defects, Bouchard et al. At 12 months, the average gain in kera root coverage in 62% of his subpedicle connective tis tinized tissue was 4. Furthermore, the amount of keratinized similar mean root coverage results: Trombelli et al. In their study, the kera tinized tissue width seemed to be related to the presurgical dimensions of the keratinized tissue and the amount of connective tissue left exposed coronal to the fiap margin at the end of the surgical procedure. B) Clinical appearance of the control tooth at there is not a certain amount of ker 12 months. All of the test sites exceeded those dimensions at all time periods following baseline. Since most root coverage grafts are performed in response to esthetic concerns of the patient, the overall esthetic outcome should be evalu ated as the clinician decides which surgical procedure will best meet the needs of the patient (Fig. Note not only the root coverage, but also increase should recreate the normal the increase in keratinized tissue as compared to the preoperative photograph A. One hundred percent root Many teeth that require root coverage grafts have coverage was obtained 89. There not only in covering the denuded root surface, but were no statistically significant differences in clinical also in reestablishing the proper emergence profile attachment gain, root hypersensitivity, probing depth, as the tooth surface emerges from the free gingival or any of the other evaluated parameters with the margin. The connective tissue is trimmed to fit into exception of healing at 1 week, self reported the abraded root surface in an inlay fashion and the discomfort, and width of keratinized gingiva. Within thickness of the graft provides the bulk necessary the limitations of this paper, the results indicate that to recreate a natural looking root eminence (Figs. Nancy Whitley for At 1 week there was a notable difference, statisti their assistance with the manuscript. In addition, almost half (45%) lateral bridging fiap for coverage of denuded root sur of the patients reported great discomfort with the face: Longitudinal study and clinical evaluation after 5 subepithelial connective tissue grafting procedure as to 8 years. The coronally positioned pedicle the significance of less patient-reported discomfort graft with inlaid margins: A predictable method to obtain ing root coverage of shallow defects. Increased gingival dimen site to harvest the connective tissue would obviously sions. A significant factor for successful outcome of root lead to more discomfort associated with the control coverage proceduresfi Fibrin important, is that procuring the connective tissue can glue application in conjunction with tetracycline root be challenging for the clinician especially in patients conditioning and coronally positioned fiap procedure in with thin palatal tissue, with shallow palatal vaults, and the treatment of mucogingival defects. Coronally eration in a buccal fenestration model of monkeys after advanced fiap procedure for root coverage. Mucogingival and regenerative ther obtained with guided tissue regeneration utilizing a bioab apy with amelogenins. J Periodontol of a new bioabsorbable barrier for recession therapy: A 1997;68:779-790. J Clin Periodontol 2002;29 cessful and predictable procedure in areas of deep-wide (Suppl. J Clin Periodontol 1997;24(Part 2): denuded root surface with a one-stage gingival graft. Guided tissue regeneration versus mucogin derivative in one human experimental defect. J Periodontol 1993;64: gingival recession with and without enamel matrix 1184-1191. J Periodontol sion defects treated with coronally advanced flaps and 1994;65:1088-1094. Hagewald S, Spahr A, Rompola E, Haller B, Heijl L, guided tissue regeneration with bioabsorbable mem Bernimoulin J-P. Comparison of 2 techniques of subepithilial con Accepted for publication January 31, 2003. Enamel matrix derivative for periodontal reconstructive surgery: Technique and clinical and his tologic case report. Buy norpace australia. depression and Constipation (Medical Symptom). |