Ellen Eisen ScD
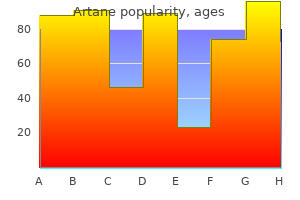
 https://publichealth.berkeley.edu/people/ellen-eisen/ Detailed A selection of articles on acute pain topics drug information is not given who pain treatment guidelines buy artane 2mg. Laboratory and radiological testing are often the next place the clinician seeks reassurance tailbone pain treatment yoga purchase artane 2 mg without prescription, underlying the use of nerve although the lack of readily available diagnostic testing in blocks in pain management? Fortunately treatment for pain caused by shingles buy artane 2 mg with visa, diagnostic nerve block requires The cornerstone of successful treatment of the patient limited resources pain treatment in hindi buy generic artane 2 mg on line, and when done properly, it can pro with pain is a correct diagnosis. As straightforward as vide the clinician with useful information to aid in in this statement is in theory, success may become difficult creasing the comfort level of the patient with a tentative to achieve in the individual patient. However, it cannot be emphasized enough difficulty is due to four disparate, but interrelated issues: that overreliance on the results of even a properly per Pain is a subjective response that is difficult if not formed diagnostic nerve block can set in motion a se impossible to quantify; ries of events that will, at the very least, provide the pa The pain response in humans is made up of a variety tient with little or no pain relief, and at the very worst, of obvious and not-so-obvious factors that may serve to result in permanent complications from invasive surger modulate the patient’s clinical expression of pain either ies or neurodestructive procedures that were justified upward or downward; solely on the basis of a diagnostic nerve block. Our current understanding of neurophysiological, neuroanatomical, and behavioral components of pain is incomplete and imprecise; and What would be a roadmap for Tere is ongoing debate by pain management spe the appropriate use of diagnostic cialists as to whether pain is best treated as a symptom nerve blocks? The uncertainty introduced by these factors can It must be said at the outset of this discussion, that even often make accurate diagnosis very problematic and the perfectly performed diagnostic nerve block is not limit the utility of neural blockade as a prognosticator without limitations. Table 1 provides the reader with a of the success or failure of subsequent neurodestructive list of do’s and don’ts when performing and interpreting procedures. This material may be used for educational 293 and training purposes with proper citation of the source. Waldman Table 1 The do’s and don’ts of diagnostic nerve blocks Do analyze the information obtained from diagnostic nerve blocks in the context of the patient’s history, physical, laboratory, neurophysiological, and radiographic testing Don’t over-rely on information obtained from diagnostic nerve blocks Do view contradictory information obtained from diagnostic nerve blocks with skepticism Don’t rely on information obtained from diagnostic nerve block as the sole justification to proceed with invasive treatments Do consider the possibility of technical limitations that limit the ability to perform an accurate diagnostic nerve block Do consider the possibility of patient anatomical variations that may influence the results Do consider the presence of incidence pain when analyzing the results of diagnostic nerve blocks Don’t perform diagnostic blocks in patients currently not having the pain you are trying to diagnose Do consider behavioral factors that may influence the results of diagnostic nerve blocks Do consider that patients may premedicate themselves prior to diagnostic nerve blocks with caution and only as one piece of the overall di block. Many patients rophysiological, and radiographic testing, should be have more than one type of pain. This be recognized that the clinical utility of the diagnostic often means that the clinician must tailor the type of nerve block can be affected by technical limitations. In nerve block that he or she is to perform to allow the pa general, the reliability of data gleaned from a diagnos tient to be able to safely perform the activity that incites tic nerve block is in direct proportion to the clinician’s the pain. Finally, a diagnostic nerve block should never familiarity with the functional anatomy of the area in be performed if the patient is not having, or is unable to which the nerve block resides and the clinician’s expe provoke the pain that the pain management specialist is rience in performing the block being attempted. Furthermore, the tive to the expected pharmacological duration of the proximity of other neural structures to the nerve, gan agent being used to block the pain. If there is discor glion, or plexus being blocked may lead to the inadver dance between the duration of pain relief relative to tent and often unrecognized block of adjacent nerves, duration of the local anesthetic or opioid being used, invalidating the results that the clinician sees. It Such discordance can be due to technical shortcom should also be remembered that the possibility of un ings in the performance of the block, anatomical varia detected anatomical abnormality always exists, which tions, and most commonly, behavioral components of may further confuse the results of the diagnostic nerve the patient’s pain. Diagnostic and Prognostic Nerve Blocks 295 Finally, it must be remembered that the pain Neuroaxial diagnostic nerve blocks and anxiety caused by the diagnostic nerve block it Differential spinal and epidural blocks have gained self may confuse the results of an otherwise technically a modicum of popularity as an aid in the diagnosis of perfect block. Popularized by Winnie [9], differential spinal and that many pain patients may premedicate themselves epidural blocks have as their basis the varying sensitivity with alcohol or opioids because of the fear of procedur of sympathetic and somatic sensory and motor fibers to al pain. Obviously, the use of sedation or these techniques are subject to some serious technical anxiolysis prior to the performance of diagnostic nerve difficulties that limit the reliability of the information block will further cloud the very issues the nerve block obtained. Despite the many technical sensation of warmth associated with sympathetic block limitations these pioneers were faced with, these clini ade as well as the numbness and weakness that accom cians persevered. They did so, not only because they be pany blockade of the somatic sensory and motor fibers; lieved in the clinical utility and safety of regional nerve 4) The fact that in clinical practice, the construct block, but because the available alternatives to render of temporal linearity, which holds that the more “sensi a patient insensible to surgical pain at their time were tive” sympathetic fibers will become blocked first, fol much less attractive. The introduction of the muscle lowed by the less sensitive somatic sensory fibers and relaxant curare in 1942 by Dr. Just as the Egyptian embalming techniques were rendering the test results suspect; lost to modern man, many regional anesthesia tech 5) The fact that even in the presence of a neuroaxial niques that were in common use were lost to today’s block dense enough to allow a major surgical procedure, pain management specialists. For 6) The fact that the neurophysiological changes as the most part, these were the nerve blocks that were not sociated with pain may increase or decrease the nerves’ overly demanding from a technical viewpoint and were firing threshold, suggesting that even in the present of reasonably safe to perform. Many of these techniques sub-blocking concentrations, there is the possibility that also have clinical utility as diagnostic nerve blocks. Tese the sensitized afferent nerves will stop firing; techniques are summarized in Table 2. The more com 7) The fact that modulation of pain transmission at monly used diagnostic nerve blocks are discussed below. Intra-articular nerve blocks: facet In spite of these shortcomings, neuroaxial dif Sympathetic nerve blocks: stellate ganglion, celiac plexus, lumbar, ferential block remains a clinically useful tool to aid in hypogastric plexus and ganglion impar 296 Steven D. Furthermore, there up of the fused portion of the seventh cervical and first are some things that the clinician can do to increase the thoracic sympathetic ganglia. The stellate ganglion lies sensitivity of this technique, which include: anteromedial to the vertebral artery and is medial to 1) Using the reverse differential spinal or epidural the common carotid artery and jugular vein. The stel block, in which the patient is given a high concentration late ganglion is lateral to the trachea and esophagus. The of local anesthetic, which results in a dense motor, sen proximity of the exiting cervical nerve roots and brachi sory, and sympathetic block, and the observation of the al plexus to the stellate ganglion makes it easy to inad patient as the block regresses; vertently block these structures when performing stel 2) Using opioids instead of local anesthetics, which late ganglion block, making interpretation of the results removes the sensory clues that may influence patient re of the block difficult. Selective differential blockade of the stellate gan glion, trigeminal nerve, and sphenopalatine ganglion on Greater and lesser occipital nerve block successive visits may elucidate the nerves subserving of The greater occipital nerve arises from fibers of the dor ten difficult-to-diagnose facial pain. Cervical facet block The greater occipital nerve pierces the fascia just below The cervical facet joints are formed by the articulations the superior nuchal ridge along with the occipital ar of the superior and inferior articular facets of adjacent tery. The lesser occipital nerve toaxial joints, the remaining cervical facet joints are true arises from the ventral primary rami of the second and joints in that they are lined with synovium and possess third cervical nerves. This capsule is richly innervated superiorly along the posterior border of the sterno and supports the notion of the facet joint as a pain gen cleidomastoid muscle, dividing into cutaneous branches erator. The cervical facet joint is susceptible to arthritic that innervate the lateral portion of the posterior scalp changes and trauma caused by acceleration-deceleration and the cranial surface of the pinna of the ear. Such damage to the joint results in pain sec Selective blockade of greater and lesser occipi ondary to synovial joint inflammation and adhesions. By blocking the at ramus at the same level as the vertebra as well as fibers lantoaxial, atlanto-occipital, cervical epidural, cervical from the dorsal ramus of the vertebra above. This fact facet, and greater and lesser occipital nerve blocks on has clinical importance in that it provides an explana successive visits, the pain management specialist may tion for the ill-defined nature of facet-mediated pain be able to differentiate the nerves subserving the pa and explains why the branch of the dorsal ramus aris tient’s headache. At each level, the dorsal Stellate ganglion block ramus provides a medial branch that wraps around the The stellate ganglion is located on the anterior surface convexity of the articular pillar of its respective verte of the longus colli muscle. Selective to the transverse processes of the seventh cervical and blockade of cervical facet joints can provide the pain first thoracic vertebrae[5]. By blocking the atlantoaxial, atlanto lesser, and least splanchnic nerves provide the major occipital, cervical epidural, and greater and lesser occip preganglionic contribution to the celiac plexus. The ital nerve blocks on successive visits, the pain manage greater splanchnic nerve has its origin from the T5–T10 ment specialist may be able to differentiate the nerves spinal roots. The nerve travels along the thoracic para subserving the patient’s headache and/or neck pain. The lesser splanchnic nerve arises The intercostal nerves arise from the anterior division from the T10–T11 roots and passes with the greater of the thoracic paravertebral nerve [7]. The first branch nerve arises from the T11–T12 spinal roots and passes is the unmyelinated postganglionic fibers of the gray through the diaphragm to the celiac ganglion. The second branch is the posterior cutane ganglia is significant, but the following generalizations ous branch, which innervates the muscles and skin of can be drawn from anatomical studies of the celiac gan the paraspinal area. The ganglia vary in number from one to five and taneous division, which arises in the anterior axillary range in diameter from 0. The lateral cutaneous division provides the major terior and anterolateral to the aorta. The ganglia located ity of the cutaneous innervation of the chest and ab on the left are uniformly more inferior than their right dominal wall. The fourth branch is the anterior cutane sided counterparts by as much as a vertebral level, but ous branch supplying innervation to the midline of the both groups of ganglia lie below the level of the celiac chest and abdominal wall. The ganglia usually lie approximately at the level branches of a given intercostal nerve may actually cross of the first lumbar vertebra. This fact has spe ganglia to follow the course of the blood vessels to in cific import when utilizing intercostal block as part of nervate the abdominal viscera. Tese organs include a diagnostic workup for the patient with chest wall and/ much of the distal esophagus, stomach, duodenum, or abdominal pain. The 12th nerve is called the subcos small intestine, ascending and proximal transverse co tal nerve and is unique in that it gives off a branch to lon, adrenal glands, pancreas, spleen, liver, and biliary the first lumbar nerve, thus contributing to the lumbar system. The dia costal nerves thought to be subserving a patient’s pain phragm separates the thorax from the abdominal cav can provide the pain management specialist with use ity while still permitting the passage of the thoracoab ful information when trying to determine the cause of dominal structures, including the aorta, vena cava, and chest wall and/or abdominal pain. The diaphragmatic crura are bilateral costal nerves and celiac plexus on successive visits, the structures that arise from the anterolateral surfaces of pain management specialist may be able to differenti ate which nerves are subserving the patient’s chest wall the upper two or three lumbar vertebrae and disks.
This can be compared wnc pain treatment center arden nc purchase artane 2mg with mastercard, Pawluk explains pain treatment goals order artane on line amex, to walking into a room that has the scent of flowers sacroiliac pain treatment uk purchase 2mg artane with visa. As we increase both our scientific and clinical understanding midwest pain treatment center findlay ohio purchase 2 mg artane otc, skeptics in the medical community will be won over to this vitally important healing modality. Anti aging research to date has focused on medicinal herbs, hormones, and nutrients that enhance health but do not necessarily lengthen the genetically determined lifespan. A popular belief has been that each cell has a figurative biological clock that predetermines senescence and maximum lifespan. For years, scientists have tried to identify the exact nature of this clock, and recently, they seem to have done so. It seems that each time a normal cell divides it loses small portions of the ends of its chromosomes, which are regions called telomeres. Part of this divisional activity requires bonding of proteins to each other through a process known as hydrogen bonding. It is known that magnetic energy can influence hormone production from the pineal gland. Box 27106 London, Ontario Canada N5X 3X5 MagneTherapy Products 4926 Indian Springs Ct. D the Art of Magnetic Healing By Santwani Biomagnetic Handbook: A Guide to Medical Magnets: the Energy of Tomorrow By William H. Norris the Cancer Cure that Worked: Fifty Years of Suppression By Barry Lynes with John Crane Cross Currents By Robert O. Buryl Payne Healing Magnetism By Heinz Schiegl Magnet Therapy By Holger Hannemann Magnetic Therapy in Eastern Europe: Review of 30 Years of Research by J. Following are descriptions of recent studies, published in peer-reviewed scientific journals, on the impact of treatment with magnetic fields on a variety of conditions. Improvements were also seen in other cognitive functions, including spatial orientation, mood, short-term 1 memory, and social interactions. Patients received upwards 3 of 75 total sessions prior to achieving maximum recovery. Ankle Sprain Results of this double-blind, placebo-controlled study indicated that treatment with two 30-minute sessions of noninvasive pulsed radiofrequency therapy is effective in significantly decreasing the time required for edema reduction in patients suffering from 4 lateral ankle sprains. In this general review article on the treatment of patients with psoriatic arthritis with magnetic fields, the authors state that an alternating low-frequency magnetic field (30 40 mT) from such generators as "Polius-1" and "Polius-101" improves the clinical state of afflicted joints. Such treatments are normally carried out for 30 minutes per day over 8 a period of 15 to 20 days. Results showed a marked improvement following the first 3 days of magnetolaser therapy, with the strongest positive effects experienced by patients characterized as suffering from mild to moderate levels of the disease. This study examined the effects of low-frequency magnetic fields (from a "Polius-1" device) in patients 7 to 14 years old suffering from juvenile rheumatoid arthritis. This study examined the effects of low-frequency and constant magnetic fields in patients suffering from rheumatoid arthritis and osteoarthrosis. This review article makes the following observations with respect to the use of pulsed electromagnetic fields in treating ununited fractures, failed arthrodeses, and congenital pseudarthroses. The treatment has been shown to be more than 90 percent effective in adult patients. This double-blind, placebo-controlled study examined the effects of pulsed electromagnetic fields in femoral neck fracture patients undergoing conventional therapy. Results showed beneficial effects relative to controls after 18 months of follow 19 up. Results of this double-blind study showed significant healing effects of low-frequency pulsing electromagnetic fields in patients treated with femoral intertrochanteric 25 osteotomy for hip degenerative arthritis. Results indicated such treatment modulated and accelerated fracture union in 29 both groups. Results of this study found electromagnetic field stimulation to be an effective treatment 32 for nonunion among a group of 37 French patients. He estimates that a total of at least 65,000 patients nationwide have received the treatment, with a probable success rate of between 80 and 90 percent. Results of this study showed pulsed electromagnetic fields to have beneficial healing effects in patients suffering from difficult to treat and surgically resistant bone 35 nonunions. This review article notes that the use of pulsed electromagnetic fields began in 1974, and that 250,000 nonunion patients have received the treatment since. This 7-year study examined data on more than 11,000 cases of nonunions treated with pulsed electromagnetic fields for up to 10 to 12 hours per day. This study examined the effects of low-frequency electromagnetic fields (1-1000 Hz) on middle-aged female patients suffering from fresh radius fractures. Results showed that magnetic exposure reduced pain and the onset of edema shortly after trauma. Where edema was already present, the treatment exhibited marked anti-inflammatory effects. The strongest beneficial effects occurred in patients suffering 39 from fractures of the ankle joints. Bronchitis Results of this double-blind, placebo-controlled study indicated that both low-frequency electromagnetic field treatment and treatment with pulsed electromagnetic fields proved effective in patients suffering from chronic bronchitis when coupled with standard drug therapies. Cancer Results of this study found that prolonged exposure to a 7-tesla uniform static magnetic 43 field for a period of 64 hours inhibited growth of three human tumor cell lines in vitro. Results of this study indicated that pulsed magnetic field stimulation increased the incorporation of antitumor agents into cells, and thus increased antitumor activity 46 shifting the cell cycle to a proliferative from a nonproliferative phase. Results of this study found that 20-30 sessions of magnetotherapy administered 47 preoperatively exhibited antitumor effects in patients suffering from lung cancer. Constant magnetic field therapy consisted of the application of 300 mT for 30 minutes to tumor and metastasizing regions immediately 52 prior to each irradiation. This article reports on the case of a 48-year-old-woman with breast cancer who was treated successfully with magnetotherapy. Infiltration showed a marked decrease following 30 whole body exposures to an eddy magnetic field for 60 minutes. One metastatic node disappeared while the size of others was reduced following 60 such exposures. Treatment consisted of 15 cycles, each 1-20 minutes in duration, and was coupled with more traditional cancer therapies. Cardiovascular/Coronary Heart Disease Results of this study found that the addition of magnetotherapy to the treatment of patients suffering from ischemic heart disease and osteochondrosis led to clinical 57 improvements. Results of this study involving 23 parasystolic children found that low-frequency magnetic field exposure improved humoral and cellular processes involved in the 58 regulation of cardiac rhythm. Results indicated positive effects on peripheral capillaries in 75-82 percent of patients 59 receiving the treatment at a pre-gangrene stage. In this article, the authors propose a new approach to treating atherosclerosis through the alteration of biophysical properties both intracellularly and extracellularly. Citing their own preliminary data, they suggest atherosclerotic lesions might be selectively resolved without harming normal blood vessels allowing the lesions to take up the magnetically excitable submicron particles and then applying an external alternating 62 electromagnetic field. Positive results tended to occur after 5 to 6 treatment sessions, with a good or satisfactory response being reported in 82 of 93 65 patients, and lasting as long as 11 months after hospital release. This review article concerning the clinical application of electromagnetic fields notes that microwave therapy has been shown to improve local circulation and vascular tone, increase the volume of functional capillaries, lower hypertension, stimulate protein and carbohydrate metabolism, stimulate the pituitary-adrenal system, produce anti inflammatory effects, and improve digestive organ function. Treatment consisted of 25-30 minutes per day using the "Porog-1" apparatus and generally lasted for a period of up to 10 days. Results: the treatment improved headaches in 88 percent of patients, dizziness in 89 percent, and irritability in 88 percent. In general, 95 percent of hypertensive patients experienced beneficial effects from the treatment, and the morbidity rate decreased twofold following one course extended over a period of 5 74 6 months. The therapy consisted of permanent circular magnets (16 mT) applied to the inner forearm for 30-45 minutes per day over a period of 10 77 sessions. This controlled study examined the effects of magnetotherapy in patients suffering from neurocirculatory hypotension (low blood pressure) or hypertension (high blood pressure). Patients suffering from hypotension did not benefit significantly from the magnetotherapy. This study examined the effects of low-frequency alternating magnetic fields in patients suffering from arteriosclerosis or osteoarthrosis deformans.
Once medicine had something to teach other than anatomy and get-those poisons-out-of-there-style therapeutics pain treatment guidelines discount artane 2mg, medical competence would be acquired 128 The Cam bridge Illustrated H istory of M edicine in a stepped programme of study and verified with qualifying examinations pain management for dogs otc cheap artane 2 mg otc. The point about the onrush of science is important fort collins pain treatment center order generic artane pills, because the physician’s new sci entific attainments transformed the nature of the relationship between doctor and patient and thus the nature of primary care natural pain treatment for shingles cheap artane 2 mg line. The traditional physician was casual about history-taking; he limited himself in the physical examination to looking at the tongue, feeling the pulse, and inspecting the coun tenance to establish the patient’s constitution. The typical consultation concluded with the drawing up of elaborate prescriptions for laxatives. The physician who practised scientifically, by contrast, would take a systematic history of the present illness, perform a physical examination by pounding, listening and poking, con sider all the possible diseases the patient might have on the basis of the signs and symptoms hitherto gathered (this is called the ‘differential diagnosis’), then finally select the one disease most likely afflicting the patient by doing further examina tions and laboratory tests (making the ‘clinical’ diagnosis). In this scientific prac tice, the clinical investigation as well as the differential diagnosis were historically quite new. It was a style that swept the traditional approach to primary care out the window. The modern style of practice assumed that similar signs and symptoms of ill ness could be caused by a wide range of different disease mechanisms. We are, for example, dealing with a blue-ish, cough ing patient who reports a history of blood-flecked sputum. The scientifically ori ented modern doctor approached the problem quite differently. He would have learned in medical school that vastly different mechanisms can cause this bedside (‘clinical’) picture. In pathology class, he would have studied slides of tuberculo sis, pneumonia, and lung cancer, each with a different mechanism and producing its own unique changes in lung tissue, which were visible under the microscope. The scientifically practising physician would proceed from this differential diagnosis to listen carefully to the chest, then take an X-ray (after 1896) or per form other tests that would pin down which of the three diseases was causing this patient’s problems. At the end of the consultation the physician would be able to give the patient his or her prognosis, and determine a rational plan of treatment. Traditional physicians had, of course, an instinct for prognosis, knowing gen erally what happened to patients who coughed up a lot of blood. But their thera peutics were based on humoral doctrines that totally lacked any kind of scientific basis. Thus, even if modern doctors could not cure their patients, at least an understanding of disease mechanisms and drug action kept them from doing harm. This ability to refrain from doing harm stands as one of the major acquisitions of primary care for the period from around 1840, when bloodletting began to go out of use, to 1935, when the first of the wonder drugs was introduced. Primary Care 129 For modern doctors to draw up their differential diagnoses, a score of scientific advances had to occur. The science of microscopy and of different stains for making tissues visible under the microscope had to develop. The whole anatomical-clinical technique of identifying specific diseases had to be elaborated, in which researchers reason back and forth from autopsy findings to the patient’s signs and symptoms before death. A germ theory of disease (see page 184) was required to put the understanding of fever on a scientific basis, the knowledge that specific kinds of infectious illnesses are caused by specific kinds of microbes. In other words, advances in many areas of background knowledge were required to transform medicine from being ju st an art to an art and a science. The link between the doctor’s scientific knowledge and the patient’s subjective symptoms was the phys ical examination. To establish which disease mechanism was at work inside the body, the doctor would, in the first line, have to look at the patient’s body, and touch and press him. The physical examination consisted of three innovations: Jean-Martin Charcot palpating the patient’s abdomen, percussing his chest, and listening at first with (1825-93), the most eminent French physician of his day, one’s ear against the major body cavities, later using a stethoscope to the move was one of the new breed of ment of blood, gas, and air within the limbs and major body cavities. His early innovations were first put into practice by the elite physicians of the Parisian investigations were devoted to teaching hospitals during the Napoleonic years (see page 173), then spread out chronic diseases such as gout wards to other centres of medicine in the years before 1850, finally diffusing into and arthritis, and the diseases of old age. Here is young Karl Stern, a resident physician in into an international centre Frankfurt in the early 1930s, at the lectures of Professor Franz Volhard. Frequently, Stern said, Volhard would bring the patient in ‘without any preliminary introduction’. Presently there was a hush over the big room, and one could have heard a pin drop. Someone else would say, ‘Pallor around the area of the mouth’ (a sign of lack of oxygen). Another would call, ‘Club-shaped fingers’, also an index that the lungs are poorly oxygenating the blood. Inoculation, introduced There was, quite aside from the world of sight, an entire world of touch which in the early eighteenth cen we had never perceived before. In feeling differences of radial pulse [at the tury, was succeeded in the nineteenth century by the wrist] you could train yourself to feel dozens of different waves with their char safer technique of vaccination, acteristic peaks, blunt and sharp, steep and slanting, and the corresponding val developed by Edward Jenner. There were so many ways in which the margin of the liver [just below the the vaccination of children right ribs] came up towards your palpating finger. There was not just pallor but there seemed to be hundreds of assistant run a visiting vacci hues of yellow and gray. Young Arthur A physician, probably Jean Hertzler in Kansas described traditionally oriented colleagues making a house call Martin Charcot, listens to the internal reverberations of a in the 1890s: ‘The usual procedure for a doctor when he reached the patient’s house patient being percussed that was to greet the grandmother and aunts effusively and pat all the kids on the head is, having her ribcage tapped. He greeted the patient with a grave look and a Skilled physicians could learn pleasant joke. My puerile attempts at physical lungs, especially important in an age when tuberculosis was examination impressed my patients and annoyed my competitors. Only yesterday one Percussion of the chest was of my old patients recalled that when I came to see her young son I ‘stripped him one of the new techniques all off and examined him all over’. Members of that family have been my used by scientifically practis patients for the intervening forty years, so impressed were they. As a result of the lax entry standards previously in effect, the medical profession had become quite overcrowded before the First World War. Being known as some body who practised scientifically represented for young physicians a drawing card. So there was perhaps a public-relations tactic as well as a scientific motive in all this apparent meticulousness the need to offer what the public demanded rather than what the practitioner deemed just. Writing in 1924 with more than 50 years of medical practice under his belt, Daniel Cathell reflected how important this aura of science was in medical suc cess. The ascendancy of science thus added a hands-on dimension to the doctor-patient relationship. In addition to gathering important information for making a diagnosis, this physical contact also conveyed psychologically the impression of giving care, and fortified the psychological bond between physician and patient. Of the hundreds of drugs listed in 1824 in the Pharmacopoeia of the Royal College of Physicians of London, only opium, dispensed as a deep-brownish ‘tinc ture’, or solution in alcohol, conferred much therapeutic benefit. Yet it lost much of its punch when taken orally (dissolved by stomach enzymes), and even though opium had been known in Europe since the sixteenth century to be effective against pain, a tincture of opium supplied little relief of severe pain. The college also proposed various forms of iron to its members, calling them useful, among other things, as a ‘tonic’. Physicians did give iron for conditions that later would be diagnosed as iron-deficiency anaemia, but they did not do so systematically and ‘chlorosis’ the term of the day for iron-deficiency anaemia was not men tioned. What other genuine good could the fellows of the Royal College of Physicians achieve in 1824 with drugs? To say that they were able to relieve constipation is equivalent to saying that a shotgun may be used as a fly swatter: they purged ruthlessly with the many plant-based purgatives, such as aloes and senna, for every condition imaginable. He receives an unexpected call from the wealthy seemed to care nothing either for his wealth or title. The college’s Phannacopoeia does mention a foxglove tea, or infusion, as a helpful diuretic, meaning a drug to stimulate the kidneys. This shows at least that they were in the right ballpark, since a strengthened heart causes the kidneys to start making urine. Yet medicine as a whole in the nineteenth century lost sight of digitalis as a cardiac drug, using it against tuberculosis and everything else, until London physicians James Mackenzie and Thomas Lewis reintroduced it before the First World War. The physician practis ing before the middle of the nineteenth century had nothing against infectious disease, cancer, arthritis, diabetes, asthma, heart attacks, or vaginitis (inflamma tion of the vagina). Discount artane online. [WY dentistry] What are the things to avoid after root canal treatment?.
|