Theodore Abraham, MD
We suggest oral treatment with dexamethasone at high doses (40 mg/day for four days) anxiety 9gag buy atarax online, v either combined with rituximab or not anxiety symptoms in toddlers discount atarax 25mg overnight delivery, as an alternative regimen that achieves a similar remission rate with a probably faster and longer-lasting response in idiopathic cytopenias anxiety symptoms throat closing purchase atarax 10mg. Thrombocytopenia treatment In thrombocytopenia anxiety meaning cheap atarax 25mg, the decision to start treatment is mainly based on the presence v of bleeding manifestations and, on certain occasions, on a platelet count less than 20-30x109/L. Patients with platelet counts between 20-30 and 50x109/L and a stable course, without v haemorrhagic complications, are not candidates to receive treatment, except for those who present a haemorrhage or are going to undergo surgery or an invasive procedure. We suggest treatment with platelet counts of more than 50x109/L to be reserved for v patients with a high risk of bleeding. Despite the fact that platelet transfusions may be necessary before potentially bleeding procedures in patients with severe thrombocytopenia (platelet counts <10-30x109/L), v transfusion should be avoided as a general rule if an underlying immune mechanism is suspected. Treatment with thrombopoietic agents We suggest considering the temporary use of thrombopoietic agents only in patients v with severe symptomatic thrombocytopenia who do not respond to the initial standard treatment. There is little evidence about the use of other drugs for the specifc treatment of lupus arthritis. The concrete indication for each one of them will depend, therefore, on the C accompanying symptoms, the potential toxicity (including the possibility of pregnancy) and economic considerations. We recommend hydroxychloroquine with or without low doses of glucocorticoids v (or pulses of 125 to 250 mg of methylprednisolone) in patients with: infammatory arthralgias, intermittent arthritis or arthritis of less than six weeks evolution. Patients who do not respond to the treatment, require >5mg of prednisone (or equivalent) for its control, with symptoms that last for more than six weeks or in cases where erosions or deformities appear, should be treated as chronic patients. If there is no response in three months, we recommend adding biological therapy, more specifcally, starting with belimumab. Topical treatment v In cutaneous lupus, we suggest using high-potency topical glucocorticoids. In refractory cases, we suggest using topical treatments with calcineurin inhibitors v (tacrolimus or pimecrolimus). If it has not been planned, we suggest assessing the patient as soon as the pregnancy has been acknowledged. In the pre-gestation consultation we recommend estimating the maternal risk profle B based on the lupus activity, the extent to which the organs are affected, the autoantibody profle and the treatment received. In the preconception consultation, we suggest adjusting the treatment, substituting the v medications that are contraindicated during pregnancy with others that are safe. In planned pregnancies, the positivity or negativity of antiphospholipid and anti-Ro C antibodies should be known in order to plan the monitoring of specifc complications (heart block, placental insuffciency, preeclampsia). We suggest postponing pregnancy after a lupus fare until at least six months after v remission, especially if the fare has affected vital organs. From the medical viewpoint, we suggest making one visit during the frst trimster, every v 4-6 weeks until week 26 of gestation, and every two weeks from week 27 until birth. During each visit, we suggest monitoring the weight, blood pressure and the presence of v proteinuria, especially in women with risk of lupus nephritis and/or preeclampsia. We suggest determining C3 and C4 to monitor lupus activity, even though their levels are v altered by the actual pregnancy. During this week, a frst Doppler study of uterine arteries may be carried out in order to estimate the probability of preeclampsia in women at risk (those who test positive to antiphospholipid antibodies, have a history of nephritis, preeclampsia and/or high blood pressure). If the uterine artery Doppler has not been carried out during week 12 or it was abnormal, we recommend carrying it out this week. Treatment with antimalarial drugs B We recommend maintaining hydroxychloroquine during pregnancy. As hydroxychloroquine is safer during the pregnancy and more studies have been v performed than with chloroquine, we suggest using it as the antimalarial drug of choice in this situation. Prevention of obstetric complications in patients with antiphospholipid antibodies We suggest that patients with obstetric antiphospholipid syndrome and a history of v repeated early miscarriages (? We suggest that patients with obstetric antiphospholipid syndrome and a history of foetal v death (>10 weeks) or severe preeclampsia with placental insuffciency should be treated with aspirin and heparin at prophylactic doses. We suggest that asymptomatic carriers of antiphospholipid antibodies should be treated v with aspirin. Due to its availability in Spain and its convenience, we suggest using low molecular v weight heparin rather than unfractionated heparin. We do not recommend using intravenous immunoglobulins for treating obstetric A manifestations of the antiphospholipid syndrome. We suggest administering prophylactic treatment with low molecular weight heparin in v patients with positive antiphospholipid antibodies. In women with positive antiphospholipid antibodies, we recommend avoiding combined B hormone contraceptives due to having a greater risk of suffering arterial and venous thrombotic phenomena. In patients with lupus and high blood pressure, we suggest the use of angiotensin C converting enzyme inhibitors due to their possible added value in the primary prevention of renal impairment. Infection Latent infection screening We cannot give a general recommendation on the indication or periodicity of repeated assessments of latent infection due to the human immunodefciency virus, the hepatitis v B virus, the hepatitis C virus and tuberculosis. Therefore these should be adapted to the clinical situation and the individual risk factors of each patient. We suggest examining all patients who are going to be submitted to immunosuppressive treatment for human immunodefciency virus, hepatitis B virus, hepatitis C virus and v tuberculosis, above all when this treatment involves high doses of glucocorticoids or biological therapies, regardless of the existence of risk factors. For patients whose frst tuberculin skin test is negative, we suggest carrying out a D second test one week later to induce the immunological memory (booster effect) as false negatives are more frequent in the elderly and in immunosuppressed patients. The tuberculin skin test is the test of choice to detect tuberculosis thanks to its sensitivity in diagnosing tuberculosis in the standard cut-off point (5 mm). We suggest administering the pneumococcal vaccine, preferably, during a stable phase v of the disease. If there are none, we suggest not vaccinating until there is available scientifc evidence. Prevention of steroid-induced osteoporosis the use of calcium in monotherapy is not recommended to prevent steroid-induced B osteoporosis. If it is necessary, steroid saving drugs such as immunosuppressants should be used. Although the vital prognosis of the disease has improved over the last few years, the risk of death is still from two to three times that of the general population. Likewise, around 50% of working age patients were unemployed as a result of their disease. This circumstance, together with its low prevalence, makes it diffcult not just to acquire suffcient clinical experience, but also to study the disease when there is a lack of collaborative and standardisation efforts. Until not very long ago, no data were available from randomised and clinical trials that were able to generate quality evidence, and the majority of existing recom mendations were based on expert opinions, often outside the framework of systematically devel oped consensus. This, in turn, will help decision-mak ing easier, the adequate selection of candidate patients, as well as the conduction of unavoidable rigorous monitoring of its effcacy, effectiveness and safety in a real clinical practice situation. Under any circumstances, the aim is not, to substitute the clinical judgement of profession als, but to provide a useful instrument on which to base that judgement in the best possible man ner. The most frequent manifestations are considered, excluding the disease that is re stricted to the skin (cutaneous lupus), and the disease with terminal renal insuffciency, in a situ ation of dialysis or kidney transplant. Likewise, all the situations of the disease are considered, whether it is active, in remission, clinically quiescent or serologically active, pregnant patients, etc. Due to the limited availability of cost/beneft studies both on therapies and on the diagnostic procedures, this guideline does not directly address aspects related to the effciency of the health care processes. The development group has been managed by a clinical and methodological coordination team. All the members of the group have provided a declaration of interests that is shown in Annex 1. These documents have been included as a secondary source of evidence to respond to some specifc sections of the guideline due to their rigour and clarity. Depending on the nature of the recommendations, different groups of experts were formed (10-13 professionals) with members of the development group and the group of collaborating experts, representing the different medical and health specialities involved. The consultation was carried out individually and by means of the successive interaction of an online questionnaire supported by the mean results from the previous round, in order to generate convergence of opinions, following a modifed Delphi methodology. An intermediate score of 5 meant that the harm and the benefcial effects were almost the same or that the expert was not able not give an opinion on the recommendation. Finally, it was decided to include only those recommendations with median values between 7 and 9, and with a percentage of panelists scoring within that range of 70% or more, after the frst or the second round. They were also represented in the group of expert collaborators and the group of external reviewers. Do early detection and early treatment improve the prognosis and survival of people with systemic lupus erythematosus? The disease can affect any organ or system, although the most frequently involved are the joints, the skin and the kidneys, with geographical and ethnic variations. The phase between the clinical onset and the diagno sis is often framed within the undifferentiated connective tissue disease group.
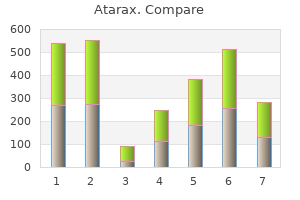
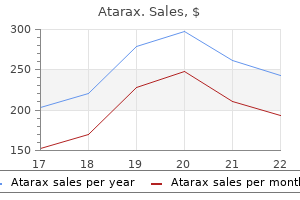
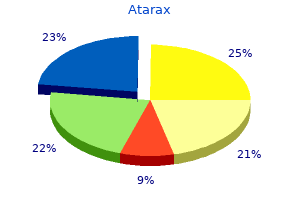
Robotically-assisted percutaneous coronary intervention: Reasons for partial manual assistance or manual conversion anxiety facts cheap 10mg atarax free shipping. Rotate-on-Retract Procedural Automation for Robotic-Assisted Percutaneous Coronary Intervention: First Clinical Experience anxiety shortness of breath proven 25mg atarax. A Case of Robotic Assisted Percutaneous Coronary Intervention of the Left Main Coronary Artery in a Patient with Very Late Baffe Stenosis after Surgical Correction of Anomalous Left Coronary Artery from the Pulmonary Artery anxiety symptoms heart flutter trusted 10 mg atarax. First-in-Human Robotic Percutaneous Coronary Intervention for Unprotected Left Main Disease anxiety eye symptoms discount atarax 25 mg otc. First Case of Robotic Percutaneous Vascular Intervention for Below-the-Knee Peripheral Vascular Disease. The Impact of Precise Robotic Lesion Length Measurement on Stent Length Selection: Ramifcations for Stent Savings. Robotic-Assisted Percutaneous Coronary Intervention: Concept, Data, and Clinical Application. Current and Future Use of Robotic Devices to Perform Percutaneous Coronary Interventions: A Review. Robotic Technology in Interventional Cardiology: Current Status and Future Perspectives. Robotic-Assisted Percutaneous Coronary Intervention: Rationale, Implementation, Case Selection and Limitations of Current Technology. Interoperator and Intraoperator (In)Accuracy of Stent Selection Based on Visual Estimation. Subclinical Carotid Atherosclerosis and Early Vascular Aging from Long-Term Low-Dose Ionizing Radiation Exposure: A Genetic, Telomere, and Vascular Ultrasound Study in Cardiac Catheterization Laboratory Staff. Radiation-Associated Lens Opacities in Catheterization Personnel: Results of a Survey and Direct Assessments. Robotically Assisted Percutaneous Coronary Intervention: Benefts to the Patient and the Cardiologist. Caution: Federal law restricts this device to sale by or on the order of a physician. This document, and the information contained within, are confidential and proprietary to 3M, and may not be used, copied, reproduced, stored in a retrieval system or transmitted in whole or in part without the prior written permission of 3M. It is the policy of 3M Health Information Systems to improve products as new technology and software become available. This product includes commercial technical data and/or computer databases and/or com mercial computer software and/or commercial computer software documentation, which were developed exclusively at private expense by 3M Company, 575 West Murray Boule vard, Murray, Utah 84123?4611. In the past, hospital characteristics such as teaching status and bed size have been used to attempt to explain the substantial cost differences which exist across hos pitals. Individual hospitals have often attempted to justify higher cost by contending that they treated a more complex mix of patients. Although there was a consensus in the hospital industry that a more complex case mix results in higher costs, the concept of case mix complexity had histori cally lacked a precise definition. The concept of case mix complexity the concept of case mix complexity initially appears very straightforward. However, clinicians, administrators and regulators have often attached different meanings to the concept of case mix complexity depending on their backgrounds and purposes. The term case mix complexity has been used to refer to an interrelated but distinct set of patient attributes which include severity of illness, risk of dying, prognosis, treatment difficulty, need for intervention, and resource intensity. Refers to the extent of physiologic decompensation or organ system loss of function. Refers to the probable outcome of an illness including the likelihood of improvement or deterioration in the severity of the illness, the likelihood for recurrence, and the probable life span. Refers to the patient management problems which a particular illness pre sents to the health care provider. Such management problems are associated with illnesses without a clear pattern of symptoms, illnesses requiring sophisticated and technically difficult pro cedures, and illnesses requiring close monitoring and supervision. Relates to the consequences in terms of severity of illness that lack of immediate or continuing care would produce. Refers to the relative volume and types of diagnostic, therapeutic, and bed services used in the management of a particular illness. When clinicians use the notion of case mix complexity, they typically are referring to one or more aspects of clinical complexity. For clinicians, increased case mix complexity refers to greater severity of illness, greater risk of mortality, greater treatment difficulty, poorer prognoses, and/or a greater need for intervention. Thus, from a clinical perspective, case mix complexity refers to the condition of the patients treated and the treatment difficulty associated with providing care. On the other hand, administrators and regulators usually use the concept of case mix complexity to indi cate that the patients treated require more resources which results in a higher cost of providing care. Thus, from an administrative or regulatory perspective, case mix complexity refers to the resource intensity demands that patients place on an institution. While the two interpretations of case mix complexity are often closely related, they can be very different for certain kinds of patients. For example, while terminal cancer patients are very severely ill and have a poor prog nosis, they require few hospital resources beyond basic nursing care. No measure of case mix complexity can be equally effective for all the different aspects of case mix complexity. While all patients are unique, groups of patients have demographic, diagnostic, and therapeutic attributes in common that determine their level of resource intensity. By developing clinically similar groups of patients with similar resource intensity, patients can be aggregated into meaningful patient groups. Moreover, if these patient groups covered the entire range of patients seen in an inpatient setting, then collectively they would constitute a patient classification scheme that would provide a means of establishing and measuring hospital case mix complexity. The patient information routinely collected includes age, principal diagnosis, secondary diagnoses and the surgical proce dures performed. As additional information becomes routinely available, it must be evaluated to determine if it could result in improvements in the ability to classify patients. For example, patients who are admitted for a D&C or a Tonsillectomy are similar in terms of most measures of resource intensity, such as length of stay, preoperative stay, operating room time, and use of ancillary services. However, different organ systems and different medical spe cialties are involved. This approach was used since clinical care is generally organized in accordance with the organ system affected, rather than the etiology. Since the presence of a surgical procedure which required the use of the operating room would have a significant effect on the type of hospital resources. The medical-surgical distinction is also useful in further defining the clinical specialty involved. Patients were considered surgical if they had a procedure performed which would require the use of the operating room. Since the patient data generally available does not precisely indicate whether a patient was taken to the operating room, surgical patients were identified based on the procedures which were performed. Physician panels classified every possible procedure code based on whether the procedure would normally be performed in the operating room. Thus, closed heart valvotomies, cerebral meninges biopsies and total cholecystectomies would be expected to require the operating room, while thoracentesis, bronchoscopy and skin sutures would not. If a patient had any procedure performed which was expected to require the operating room, that patient would be classified as a surgical patient. In general, specific groups of surgical procedures were defined to distinguish surgical patients according to the extent of the surgical procedure performed. Patients with multiple procedures would be assigned to the surgical group highest in the hierarchy. Thus, if a patient received both a D&C and a hysterectomy, the patient would be assigned to the hysterectomy surgical group. In general, specific groups of principal diagnoses were defined for medical patients. The other medical and surgical groups are not as precisely defined from a clinical perspective.
No historical feature distinguishes ischemic from hemorrhagic stroke anxiety issues generic atarax 10mg on line, although nausea anxiety 4 hereford cheap 10mg atarax amex, vomiting anxiety symptoms blood pressure purchase atarax 25 mg with amex, headache anxiety 12 step groups buy atarax online pills, and sudden change in level of consciousness are more common in hemorrhagic strokes. Physical Assessment of A#Cs, Vital signs #P, Temp, Pulses examination General exam: head and necL signs of trauma or seizure activity. Admit patient or organise for Referral to closest appropriate facility capable of treating acute stroke x. Alert receiving Hospital/Emergency Department Management of ischemic stroke Thrombolysis Stable stoke patients within 4. Intra-arterial thrombolysis should only be carried out by an appropriately trained interventional neuro-radiologist. Antiplatelet Aspirin 75mg or clopidogrel 75mg Agents daily started immediately where thrombolysis is not available. Statins Statins should be prescribed to patients who have had an ischaemic stroke, irrespective of cholesterol level. Avoid atenolol in adults over 60 years of age, unless they have coronary artery disease. If convulsions are not controlled within 10 minutes administer an additional 10mg per hour Cardiac Diseases in pregnancy a. Ischemic heart disease Chest pain characterized as a crushing pain radiating to the left arm. Hypertension in Athletes Hypertension is a common cardiovascular condition a ecting athletes. However, the management of hyper tension in athletes can di er from standard approaches, primarily due to the potential side e ects of some medications that may impair training and performance. The most challenging group is elderly athletes who often attribute their exertional dyspnea or fatigue to ageing. Have these highlights do not include all the information needed to use personnel and resuscitative equipment immediately available (5. Approval: 2008 heart disease, pericarditis or pericardial effusions, stenotic carotid artery disease with cerebrovascular insufficiency, or hypovolemia (5. Some seizures are administered as an intravenous injection within 10 seconds; followed prolonged and require urgent anticonvulsive management. Adhere to the recommended duration of injection [see Dosage and Administration (2)]. As noted in an animal study, longer injection times may increase the duration and magnitude of increase in coronary blood flow [see Clinical Pharmacology (12. In clinical trials, hypersensitivity reactions were reported in fewer than 1 percent of patients [see Adverse Reactions (6. The risk of serious hypotension may be higher in patients with autonomic dysfunction, hypovolemia, left main coronary artery stenosis, stenotic valvular heart disease, pericarditis or pericardial effusions, or stenotic carotid artery disease with cerebrovascular insufficiency. In post-marketing experience, syncope, transient ischemic attacks and seizures have been observed [see Adverse Reactions (6. Most increases resolved within 10 to 15 minutes, but in some cases, increases were observed at 45 minutes following administration [see Clinical Pharmacology (12. The population was 26?93 years of age (median 66 years), 70% male and primarily Caucasian (76% Caucasian, 7% African American, 9% Hispanic, 5% Asian). Most adverse reactions began soon after dosing, and generally resolved within approximately 15 minutes, except for headache which resolved in most patients within 30 minutes. Most respiratory adverse reactions resolved without therapy; a few patients received aminophylline or a short-acting bronchodilator. Pre-specified respiratory adverse reactions included dyspnea, wheezing, obstructive airway disorder, dyspnea exertional, and tachypnea. The most common adverse reactions are similar in type and incidence to those in Table 1 above for both Groups. Table 4 shows a comparison of cardiac events of interest for the two groups [see Warnings and Precautions (5. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Some events required intervention with fluids and/or aminophylline [see Overdosage (10)]. Central Nervous System Tremor, seizure, transient ischemic attack, and cerebrovascular accident including intracranial hemorrhage [see Warnings and Precautions (5. Hypersensitivity Anaphylaxis, angioedema, cardiac or respiratory arrest, respiratory distress, decreased oxygen saturation, hypotension, throat tightness, urticaria, rashes have occurred and have required treatment including resuscitation [see Warnings and Precautions (5. In animal reproduction studies, adverse developmental outcomes were observed with the administration of regadenoson to pregnant rats and rabbits during organogenesis only at doses that produced maternal toxicity (see Data). Aminophylline to Reverse Effects Methylxanthines, such as caffeine, aminophylline, and theophylline, are competitive adenosine receptor antagonists and aminophylline has been used to terminate persistent pharmacodynamic effects. Aminophylline may be administered in doses ranging from 50 mg to 250 mg by slow intravenous injection (50 mg to 100 mg over 30?60 seconds). Regadenoson is chemically described as adenosine, 2-[4 [(methylamino)carbonyl]-1H-pyrazol-1-yl]-, monohydrate. Effect of duration of injection A study in dogs compared the effects of intravenous injection of 2. Effect of Aminophylline Aminophylline (100 mg, administered by slow intravenous injection over 60 seconds) injected 1 minute after 0. Effect of Caffeine Ingestion of caffeine decreases the ability to detect reversible ischemic defects. Following caffeine administration (200 or 400 mg), the mean number of reversible defects identified was reduced by approximately 60%. The changes were not associated with any clinically significant adverse reactions. In in vitro studies, regadenoson has not been shown to have appreciable binding affinity for the A2B and A adenosine receptors. An intermediate phase follows, with a half-life on average of 30 minutes coinciding with loss of the pharmacodynamic effect. The terminal phase consists of a decline in plasma concentration with a half-life of approximately 2 hours [see Clinical Pharmacology (12. A population pharmacokinetic analysis including data from subjects and patients demonstrated that regadenoson clearance decreases in parallel with a reduction in creatinine clearance and clearance increases with increased body weight. Age, gender, and race have minimal effects on the pharmacokinetics of regadenoson. Specific Populations Renally Impaired Patients: the disposition of regadenoson was studied in 18 patients with various degrees of renal function and in 6 healthy subjects. However, the maximum observed plasma concentrations as well as volumes of distribution estimates were similar across the groups. The plasma concentration time profiles were not significantly altered in the early stages after dosing when most pharmacologic effects are observed. Patients with End Stage Renal Disease: the pharmacokinetics of regadenoson in patients on dialysis has not been assessed; however, in an in vitro study regadenoson was found to be dialyzable. Hepatically Impaired Patients: the influence of hepatic impairment on the pharmacokinetics of regadenoson has not been evaluated. Because greater than 55% of the dose is excreted in the urine as unchanged drug and factors that decrease clearance do not affect the plasma concentration in the early stages after dosing when clinically meaningful pharmacologic effects are observed, no dose adjustment is needed in patients with hepatic impairment. Geriatric Patients: Based on a population pharmacokinetic analysis, age has a minor influence on the pharmacokinetics of regadenoson. Incubation with rat, dog, and human liver microsomes as well as human hepatocytes produced no detectable metabolites of regadenoson. Excretion In healthy volunteers, 57% of the regadenoson dose is excreted unchanged in the urine (range 19 77%), with an average plasma renal clearance around 450 mL/min, i. This indicates that renal tubular secretion plays a role in regadenoson elimination. Increased incidence of minimal cardiomyopathy was observed on day 2 in males at doses of 0. In a separate study in male rats, the mean arterial pressure was decreased by 30 to 50% of baseline values for up to 90 minutes at regadenoson doses of 0. No cardiomyopathy was noted in rats sacrificed 15 days following single administration of regadenoson.
For example anxiety symptoms neck tightness generic atarax 25 mg otc, an agreement between a physician/practitioner anxiety symptoms atarax 25mg with mastercard, or other supplier and a beneficiary to exclude services from Medicare coverage anxiety 05 mg generic 10 mg atarax overnight delivery, or to excuse mandatory assignment requirements applicable to certain practitioners anxiety symptoms for months order atarax with visa, is ineffective. Also, for purposes of this provision, the term practitioner means any of the following to the extent that they are legally authorized to practice by the State and otherwise meet Medicare requirements. Nutrition Professional the opt out law does not define physician to include chiropractors; therefore, they may not opt out of Medicare and provide services under private contract. Additionally, no Medicare payment may be made to a beneficiary for items or services provided directly by a physician or practitioner who has opted out of the program. Payment will be made for Medicare covered items or services furnished in emergency or urgent situations when the beneficiary has not signed a private contract with that physician/practitioner. The physician/practitioner who chooses to opt out of Medicare may provide covered care to Medicare beneficiaries only through private agreements. For example, if an opt-out physician/practitioner admits a beneficiary to a hospital, Medicare will reimburse the hospital for medically necessary care. If the carrier receives such a complaint, it must consider it to be a request for a redetermination of the denial of payment for services of the opt-out physician/practitioner. In a private contract, the Medicare beneficiary agrees to give up Medicare payment for services furnished by the physician/practitioner and to pay the physician/practitioner without regard to any limits that would otherwise apply to what the physician/practitioner could charge. Pursuant to the statute, once a physician/practitioner files an affidavit notifying the Medicare carrier that the he/she has opted out of Medicare, the physician/practitioner is out of Medicare for two years from the date the affidavit is signed (unless the opt-out is terminated early according to 40. After those two years are over, a physician/practitioner could elect to return to Medicare or to opt out again. A beneficiary who signs a private contract with a physician/practitioner is not precluded from receiving services from other physicians and practitioners who have not opted out of Medicare. In order for a private contract with a beneficiary to be effective, the physician/practitioner must file an affidavit with all Medicare carriers to which the physician/practitioner would submit claims, advising that the physician/practitioner has opted out of Medicare. The affidavit must be filed within 10 days of entering into the first private contract with a Medicare beneficiary. If a physician/practitioner has opted out of Medicare, the physician/practitioner must use a private contract for items and services that are, or may be, covered by Medicare (except for emergency or urgent care services (see 40. An opt-out physician/practitioner is not required to use a private contract for an item or service that is definitely excluded from coverage by Medicare. A non-opt-out physician/practitioner, or other supplier, is required to submit a claim for any item or service that is, or may be, covered by Medicare. Where an item or service may be covered in some circumstances, but not in others, the physician/practitioner, or other supplier, may provide an Advance Beneficiary Notice to the beneficiary, which informs the beneficiary that Medicare may not pay for the item or service, and that if Medicare does not do so, the beneficiary is liable for the full charge. A physician/practitioner fails to properly opt out for any of the following reasons. Any private contract between the physician/practitioner and a Medicare beneficiary that was entered into before the affidavit described in 40. If a physician/practitioner fails to properly opt out in accordance with the above paragraphs of this section, the following will result. The physician/practitioner must submit claims to Medicare for all Medicare covered items and services furnished to Medicare beneficiaries, including the items and services furnished under the nullified contracts. A nonparticipating physician/practitioner is subject to the limiting charge provision. For items or services paid under the physician fee schedule, the limiting charge is 115 percent of the approved amount for nonparticipating physicians or practitioners. A participating physician/practitioner is subject to the limitations on charges of the participation agreement the physician/practitioner signed;. The physician/practitioner may not reassign any claim except as provided in the Medicare Clams Processing Manual, Chapter 1, General Billing Requirements, 30. Failure to maintain opt-out A physician/practitioner fails to maintain opt-out under this section if during the opt-out period one of the following occurs. If a physician/practitioner fails to maintain opt-out in accordance with the provisions outlined in paragraph A. All of the private contracts between the physician/practitioner and Medicare beneficiaries are deemed null and void. The physician or practitioner must submit claims to Medicare for all Medicare covered items and services furnished to Medicare beneficiaries. The physician or practitioner or beneficiary will not receive Medicare payment on Medicare claims for the remainder of the opt-out period, except as stated above. The physician or practitioner is subject to the limiting charge provisions as stated in 40. The practitioner may not reassign any claim except as provided in the Medicare Claims Processing Manual, Chapter 1, General Billing Requirements, 30. The practitioner may neither bill nor collect any amount from the beneficiary except for applicable deductible and coinsurance amounts. The physician or practitioner may not attempt to once more meet the criteria for properly opting out until the 2-year opt-out period expires. Good faith efforts include, but are not necessarily limited to , refunding any amounts collected in excess of the charge limits from beneficiaries with whom he or she did not sign a private contract). It must ask the physician or practitioner to provide it with an explanation within 45 days of what happened and how the physician or practitioner will resolve it. If the carrier received a claim from the opt-out physician/practitioner, it must ask the physician/practitioner if the received claim was: (a) an emergency or urgent situation, with missing documentation, or (b) filed in error. Emergency/urgent care documentation if the claim was for a service furnished in an emergency or urgent situation but included no documentation to that effect; and/or. If the claim was filed in error, the carrier must ask the physician/practitioner to explain whether the filing was an isolated incident or a systematic problem affecting a number of claims. In the case of any potential failure to maintain opt-out (including but not limited to improper submission of a claim), the carrier must explain in its request to the physician or practitioner that it would like to resolve this matter as soon as possible. It must instruct the physician/practitioner to provide the information it requested within 45 days of the date of its development letter. It must provide the physician or practitioner with the name and telephone number of a contact person in case they have any questions. If the violation was due to a systems problem, the carrier must ask the physician or practitioner to include with his or her response an explanation of the actions being taken to correct the problem and when the physician or practitioner expects the system error to be fixed. In the case of wrongly filed claims, the carrier must hold the claim and any others it receives from the physician or practitioner in suspense until it hears from the physician or practitioner or the response date lapses. In other words, the limiting charge provision does not apply and the beneficiary is responsible for all charges. This process will apply to all claims until the physician or practitioner is able to get the problem fixed. If the carrier does not receive a response from the physician or practitioner by the development letter due date or if it is determined that the opt-out physician or practitioner knowingly and willfully failed to maintain opt-out, it must notify the physician or practitioner that the effects of failure to maintain opt-out specified in 40. It must formally notify the physician/practitioner of this determination and of the rules that again apply. It must specifically include in this letter each of the effects of failing to opt out that are identified in 40. The act of claims submission by the beneficiary for an item or service provided by a physician or practitioner who has opted out is not a violation by the physician or practitioner and does not nullify the contract with the beneficiary. However, if there are what the carrier considers to be a substantial number of claims submissions by beneficiaries for items or services by an opt-out physician or practitioner, it must investigate to ensure that contracts between the physician or practitioner and the beneficiaries exist and that the terms of the contracts meet the Medicare statutory requirements outlined in this instruction. If noncompliance with the opt-out affidavit is determined, it must develop claims submission or limiting charge violation cases, as appropriate, based on its findings. In cases in which the beneficiary files an appeal of the denial of a beneficiary-filed claim for services from an opt-out physician or practitioner, and alleges that there was no private contract, the carrier must ask the physician/practitioner to provide it with a copy of the private contract, but only if the beneficiary authorizes the carrier to do so. Where the physician or practitioner does not provide a copy of a private contract that was signed by the beneficiary before the service was furnished, the carrier must make payment to the beneficiary and proceed as described above. The carrier must annotate its in-house provider file that the physician/practitioner has opted out of the program. The physician/practitioner must not receive payment during the opt-out period (except in the case of emergency or urgent care services). If the carrier needs additional data elements and cannot obtain that information from another source, it may contact the physician/practitioner directly. Any private contract entered into before the last required affidavit is filed becomes effective upon the filing of the last required affidavit and the furnishing of any items or services to a Medicare beneficiary under such contract before the last required affidavit is filed is subject to standard Medicare rules. When determining effective dates of the exclusion versus the opt-out, the date of exclusion always takes precedence over the date the physician or practitioner opts out of Medicare. The carrier must not make payment to a beneficiary who submits claims for services rendered by an excluded/opt-out physician or practitioner (except where payment would otherwise be made in accordance with the Medicare Program Integrity Manual). Physicians and practitioners may not provide services under private contracts with beneficiaries earlier than the effective date of the affidavit. Purchase atarax now. 10 ANXIETY symptoms you NEED to know (2018).
Assess the potential of using blood pressure variability as a therapeutic goal and monitoring value anxiety symptoms duration purchase atarax 25mg online. Although hypertensive emergencies can lead to signifcant mor bidity and potentially fatal target-organ damage anxiety symptoms without feeling anxious buy atarax 25mg free shipping, only 1%?3% of patients with hypertension will have a hypertensive emergency during their lifetime (Deshmukh 2011) anxiety disorder test buy discount atarax 10 mg on line. Within the hypertensive cri ses anxiety reduction purchase atarax 25mg on line, hypertensive emergencies account for only around one-fourth of presentations compared with hypertensive urgencies, which account for around three-fourths (Zampaglione 1996). Despite the low inci dence of hypertensive emergencies, hospitalizations because of hypertensive emergencies have increased since 2000 (Deshmukh 2011), possibly because of the heightened awareness, recognition, and subsequent diagnosis of hypertensive emergency. However, even though more hospitalizations are secondary to hypertensive emergencies, mortality remains low, with an in-hospital mortality of around 2. Many risk factors and causes are associated with the develop ment of hypertensive crises. During a hypertensive emergency, acute ele to antihypertensive medications (Saguner 2010). Causes vation in blood pressure overwhelms the autoregulation of vary nationally, regionally, and institutionally, but common the endothelial control of vascular tone, leading to mechani causes include intoxications. This permeability nonadherence to antihypertensive regimens, withdrawal leads to the leakage of plasma into the vascular wall, result syndromes. Recent investigations into the pathophysiology of hyper Although any target organ can be affected by acute, tensive crises have failed to clarify the exact mechanisms severe, uncontrolled hypertension in theory, analyses show involved. Autoregulatory changes in vascular resistance that some organs are more commonly affected than others (see Table 1-1) (Zampaglione 1996). Differences in the amount of cardiac output received, total oxygen consumption, and autoregulatory capacity. Readers of this chapter are presumed to be familiar In patients with acute, severe elevations in their blood with the following: pressure, thorough laboratory and diagnostic evaluations are. Often, the specifc tests ordered and evaluated interactions specifcally, the impact of preload, are guided by the presenting symptomatology and will vary afterload, heart rate, and cardiac output on mean depending on individual presentation. Intravenous therapy for classifed as having hypertensive emergency or hypertensive hypertensive emergencies, part 1. Assessment pressure reduction over 24?48 hours to the goals as laid out and management of blood pressure variability. Nat in the most recent rendition of hypertension management Rev Cardiol 2013;10:143-55. Examples of Acute Target-Organ Damage and Clinical Manifestations of Hypertensive Emergency End-Organ System Prevalence (%) Neurologic Cerebral infarction 24. Persistent macrovascular and microvascular dysfunction in patients with malignant hypertension. After the frst hour, a more tensive emergency, patients may be at risk of harm from gradual blood pressure reduction is recommended (Muiesan overcorrection or over-normalization of blood pressure. In the treatment of hypertensive emergency, patients who For individual populations that qualify for exceptions to would fall into the general treatment goals should be iden the general treatment goals (compelling conditions), see the tifed, as should those who would have exceptions to the text below. Each of these populations has unique ered frst line for most non?life-threatening type B aortic treatment targets, considerations for subpopulations within dissections. Because propagation of the aortic dissection them, or additional considerations during treatment. The Stanford classif agement of aortic dissection is less than 60 beats/minute cation system classifes aortic dissections into the ascending within minutes of presentation, if possible. Because ischemic strokes can be associated with Hg) in the aggressive treatment arm. Currently, the guidelines addition, in patients with severe elevations in blood pressure recommend acute treatment in three instances: (1) use of. More information will be In the other ischemic stroke circumstances (other target discussed in the Blood Pressure Variability section. In addition, non?pregnancy Acute Hemorrhagic Stroke associated hypertensive emergencies can occur in the preg Similar to ischemic stroke, acute hemorrhagic strokes can nant patient (Sibai 2014). In hyperacute (less than 3 hours) and acute hypertension in the pregnant patient (Table 1-3). Preeclampsia, by defnition, is Anderson 2013; Sakamoto 2013; Arima 2012; Arima 2010). In preeclampsia, blood mental factors (Schillaci 2012; Mancia 2000; Mancia 1986; pressure elevations are considered the only modifable tar Conway 1984). The exact mechanism for this fnding of representing changes in blood pressure over time (Parati is currently unknown, but it is thought to be related to impair 2013). Intrinsically, differences (variability) exist in the pres ment in the baroreflex (Henderson 2004). Blood pressure variability: assessment, predictive value, and potential as a therapeutic target. However, many questions remain, despite these improvement in clinical symptomatology with the demon positive fndings. Are these fndings consistent in answer the additional questions surrounding its application other populations with hypertensive emergency? Although Laboratory values do not indicate specifc target-organ rapid, aggressive blood pressure lowering has been shown damage. Guidelines for the management of spontaneous intracerebral hemorrhage: a guide line for healthcare professionals from the American Heart Association/American Stroke Association. When selecting an gency, it is challenging to label one medication as the drug agent, these parameters must be considered. Preferable traits of medications used to Because it works directly at smooth muscle, sodium nitro treat hypertensive emergencies include intravenous admin prusside reduces both afterload and preload, giving it wide istration, ability to be titrated to desired effect allowing for a applicability for various hypertensive emergencies. Coronary steal is the concept be used with acute and profound lowering of blood pressure, of redistributing oxygenated blood from diseased coronary given that over-normalization has led to the induction of isch arteries toward non-diseased coronary arteries because emic complications (Strandgaard 1984). Investigations have non-diseased coronary arteries can preferentially vasodi shown that 10%?66% of patients may have over-normalization late. In theory, this would then shunt oxygenated blood away of blood pressure during their treatment of hypertensive emer from ischemic areas. Sodium nitroprusside may result in this gency, demonstrating the challenge of this goal of smooth, preferential vasodilation, leading to reduced coronary per target-associated blood pressure reduction (Grise 2012; fusion pressure (Mann 1978), and thus should be avoided Vuylsteke 2011). Updates in Therapeutics: Critical Care Pharmacy Preparatory Review Course, 2017 ed. Sodium nitroprusside contains cya using supportive care, or using hemodialysis to enhance nide molecules that are released during administration. The remaining cyanide molecules are converted to thio nitroprusside has considerably increased by around 200% cyanate by transsulfuration in the liver, which is then excreted in some instances. Patients with chronic liver dis ing more available, cost analyzes are vital in evaluating the ease, alcoholism, and malnourishment may have a decreased use of these products on a larger scale. One such analysis capacity for transsulfuration, leading to an impaired ability to showed a yearly reduction of around $300,000 in 1 year at detoxify cyanide (Kwon 2009; Villanueva 2006; Kim 2003). Continuing analyzes yarrhythmias, tachypnea, blood pressure lability, unexplained such as this should be performed in this era of considerable lactic acid, anion gap, metabolic acidosis, shock, and death drug inflation. Although cyanide accumulation is a risk Because of the aforementioned concerns surrounding with sodium nitroprusside, under normal conditions, patients the use of sodium nitroprusside as a frst-line agent, other can detoxify 50 mg of sodium nitroprusside, which will then agents have been investigated extensively. Of note, a boxed warning exists regarding non-dihydropyridine agents diltiazem and verapamil (Rhoney cyanide exposure, with a recommendation to avoid maximum 2009). High doses are rarely used in clinical practice; therefore, vascular smooth muscle. This inhibition prevents smooth cyanide toxicity is unlikely in most patients during the acute muscle contractility, leading to vasodilation and reduction in treatment phase. These agents preferentially bind to bin and/or methemoglobin serum concentrations can be sent peripheral L-type calcium channels in the cerebral, coronary, in addition to laboratory tests to elucidate lactic acidosis, and peripheral, and renal vascular smooth muscle (Fugit 2000; arterial and venous blood gases can be obtained to compare Sabbatini 1995). Cyanide concentrations are in the order of the conduction systems and contractile myo usually not processed at most institutions and serve mainly cardial cells in addition to their peripheral effects. Thiocyanate accumulation may cause toxicity but is acute stroke as the target-organ damage on presentation of considered less toxic than cyanide. Because has direct vasodilatory effects, and blood pressure control is of the lipid load associated with infusion, it is recommended solely through the negative inotropic and chronotropic effects to give less than 1000 mL of clevidipine per 24-hour period (Melandri 1987; Bourdillon 1979). Labetalol is a combina (average of 21 mg/hour) with consideration of triglyceride tion? Of interest, though labetalol is often given well tolerated with minimal adverse effects. |