Karen M. Ayotte, MD
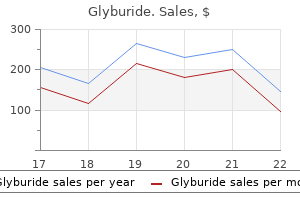
F10-F19 Mental and behavioral disorders due to psychoactive substance use with mention of: X40-X49 (Accidental poisoning by and exposure to noxious substances) can you cure diabetes in dogs order glyburide amex, code X40-X49 X60-X69 (Intentional self-poisoning by and exposure to noxious substances) blood sugar goals purchase cheap glyburide on line, code X60-X69 X85-X90 (Assault by noxious substances) diabetes walk purchase line glyburide, code X85-X90 Y10-Y19 (Poisoning by and exposure to drugs blood sugar normal range purchase glyburide 2.5mg online, chemicals and noxious substances), code Y10-Y19 Fourth character. If there is a resulting complication, consider as drug therapy and apply instructions under Y40-Y59, Drugs, medicaments and biological substances causing adverse effects in therapeutic use. F70-F79 Mental retardation Not to be used if the underlying physical condition is known. Multiple heart conditions with one heart condition specified as rheumatic: If rheumatic fever or any disease of the heart is stated to be of rheumatic origin or is specified to be rheumatic, such qualifications will apply to each specific heart condition reported (classified to I300-I319, I339, I340-I38, I400-I409, I429, I514-I519), even though it is not so qualified, unless another origin such as arteriosclerosis is mentioned. Codes for Record I (a) Acute bacterial endocarditis I330 (b) Mitral insufficiency I051 (c) Rheumatic endocarditis I091 Code to rheumatic mitral insufficiency (I051). The mitral insufficiency is coded as rheumatic since it is reported with a heart disease specified as rheumatic. Codes for Record I (a) Heart failure I099 (b) Rheumatic fever I00 Code to rheumatic heart disease (I099). Consider the heart failure to be rheumatic since it is due to rheumatic fever and there is no other heart disease on the record classifiable as rheumatic. Codes for Record I (a) Acute congestive failure I500 (b) Hypertensive myocarditis I119 (c) Rheumatic endocarditis I091 Code to hypertensive heart disease with congestive heart failure (I110). Even though rheumatic is stated on the record, it cannot be applied to the heart diseases reported. When diseases of the mitral, aortic, and tricuspid valves, not qualified as rheumatic, are jointly reported, whether on the same line or on separate lines, code the disease of all valves as rheumatic unless there is indication to the contrary. Codes for Record I (a) Mitral endocarditis I059 I051 I050 (b) insufficiency and stenosis (c) Aortic endocarditis I069 Code to disorders of both mitral and aortic valves (I080). Conditions of both valves are considered as rheumatic since the diseases of the mitral and aortic valves are jointly reported. Codes for Record I (a) Aortic and tricuspid regurgitation I061 I071 (b) Aortic stenosis I060 Code to disorders of both aortic and tricuspid valves (I082). Conditions of both valves are considered as rheumatic since the diseases of the aortic and the tricuspid valves are jointly reported. Codes for Record I (a) Mitral stenosis I050 (b) Mitral insufficiency I051 Code to mitral stenosis with insufficiency (I052). Mitral insufficiency is considered as rheumatic since it is reported jointly with mitral stenosis. If there is no statement that the rheumatic process was active at the time of death, assume activity (I010-I019) for each rheumatic heart disease (I050-I099) on the certificate in any one of the following situations: A. Rheumatic fever or any rheumatic heart disease is stated to be active or recurrent. Codes for Record I (a) Mitral stenosis I011 (b) Active rheumatic myocarditis I012 Code to other acute rheumatic heart disease (I018). Active rheumatic mitral stenosis is classified to I011 when it is reported with an active rheumatic heart disease. Therefore, the underlying cause is I018 since this category includes multiple types of heart involvement. Codes for Record I (a) Congestive heart failure I018 (b) Rheumatic fever 2 months I00 Code to other acute rheumatic heart disease (I018) since the rheumatic fever is less than 1 year duration. Codes for Record I (a) Acute myocardial dilatation I018 (b) Rheumatic fever I00 Code to other acute rheumatic heart disease (I018) since the myocardial dilatation is stated as acute. Codes for Record I (a) Acute myocardial insufficiency I012 (b) Rheumatic fever I00 Code to acute rheumatic myocarditis (I012) since the myocardial insufficiency is stated to be acute. Codes for Record I (a) Acute pericarditis I010 (b) Rheumatic mitral stenosis I011 Code to other acute rheumatic heart disease (I018) which includes multiple heart involvement since pericarditis is mentioned. Codes for Record I (a) Congestive heart failure I500 (b) Endocarditis 6 mos I011 (c) Rheumatic fever 10 yrs I00 Code to acute rheumatic endocarditis (I011) since the endocarditis is of less than 1 year duration. The term(s) in instruction E without a duration is mentioned and the age of the decedent is less than 15 years. Age 5 years Codes for Record I (a) Mitral and aortic endocarditis I011 (b) Rheumatic fever I00 Code to acute rheumatic endocarditis (I011) since the age of the decedent is less than 15 years. This classification is based on the assumption that the vast majority of such diseases are rheumatic in origin. Code these diseases as nonrheumatic if reported due to one of the nonrheumatic causes on the following list: When valvular heart disease (I050-I079, I089 and I090) not stated to be rheumatic is reported due to: A1690 C73-C759 E804-E806 J030 A188 C790-C791 E840-E859 J040-J042 A329 C797-C798 E880-E889 J069 A38 C889 F110-F169 M100-M109 A399 D300-D301 F180-F199 M300-M359 A500-A549 D309 I10-I139 N000-N289 B200-B24 D34-D359 I250-I259 N340-N399 B376 D440-D45 I330-I38 Q200-Q289 B379 E02-E0390 I420-I4290 Q870-Q999 B560-B575 E050-E349 I511 R75 B908 E65-E678 I514-I5150 T983 B909 E760-E769 I700-I710 Y400-Y599 B948 E790-E799 J00 Y883 C64-C65 E802 J020 Code nonrheumatic valvular disease (I340-I38) with appropriate fourth character. Mitral insufficiency is considered as nonrheumatic since it is reported due to Goodpasture syndrome (M310) by Rule 1. Consider diseases of the aortic, mitral, and tricuspid valves to be nonrheumatic if they are reported on the same line due to a nonrheumatic cause in the previous list. Similarly, consider diseases of these three valves to be nonrheumatic if any of them are reported due to the other and that one, in turn, is reported due to a nonrheumatic cause in the previous list. Codes for Record I (a) Mitral stenosis and aortic stenosis I342 I350 (b) Hypertension I10 Code to mitral stenosis (I342). Conditions of both valves are considered as nonrheumatic since they are reported due to hypertension (I10). Codes for Record I (a) Mitral disease I349 (b) Aortic stenosis I350 (c) Arteriosclerosis I709 Code to aortic (valve) stenosis (I350). Consider mitral disease as nonrheumatic since it is reported due to aortic stenosis which is, in turn, reported due to arteriosclerosis (I709). Codes for Record I (a) Congestive heart failure I500 (b) Mitral stenosis I342 (c) Congenital cardiomyopathy I424 Code to congenital cardiomyopathy (I424). Mitral stenosis is considered as nonrheumatic since it is reported due to congenital cardiomyopathy (I424). When multiple valvular diseases of nonrheumatic origin are reported on the same death certificate, the underlying cause should be selected by applying the General Principle or Rules 1, 2 or 3 in the usual way. If the cause is not stated, code to Other ill-defined and unspecified causes of mortality (R99). For mortality, the occurrence of myocardial infarction is assumed and assignment made to I21. If the cause is not stated, code to Other forms of chronic ischemic heart disease (I25. For mortality, the occurrence of cerebral infarction is assumed and assignment made to I63. J60-J64 Pneumoconiosis with mention of: A15-A16 (Respiratory tuberculosis), code J65 J81 Pulmonary edema with mention of: I50. O00-O99 Pregnancy, childbirth, and the puerperium Conditions classifiable to categories O00-O99 are limited to deaths of females of childbearing age. Always refer to the age and sex of the decedent before assigning a condition to O00-O99. Obstetric deaths are classified according to time elapsed between the obstetric event and the death of the woman: O95 Obstetric death of unspecified cause O960-O969 Death from any obstetric cause occurring more than 42 days but less than one year after delivery O970-O979 Death from sequela of obstetric causes (death occurring one year or more after delivery) the standard certificate of death contains a separate item regarding pregnancy. Any positive response to one of the following items should be taken into consideration when coding pregnancy related deaths. Pregnant at time of death Not pregnant, but pregnant within 42 days of death Not pregnant, but pregnant 43 days to 1 year before death If the third option for the previous list is marked and the decedent is greater than 54 years old, code as a pregnancy record only when there is a condition reported which indicates the person was pregnant either at the time of death or pregnant 43 days to 1 year before death. Consider the pregnancy to have terminated 42 days or less prior to death unless a specified length of time is written in by the certifier. Take into consideration the length of time elapsed between pregnancy and death if reported as more than 42 days. If an indirect maternal cause is selected as the originating antecedent cause, reselect any direct maternal cause on the line immediately above the indirect cause. If no direct cause is reported, the indirect cause will be accepted as the cause of death. If no other cause of maternal mortality is reported, code to Obstetric death of unspecified cause (O95). If no other cause of maternal mortality is reported, code to Complication of labor and delivery, unspecified (O759). This does not apply if the only other cause of perinatal mortality reported is respiratory failure of newborn (P28. If no other perinatal cause of mortality is reported, code to Condition originating in the perinatal period, unspecified (P96. If more than one perinatal cause is reported, apply the rules for conflict in linkage in selection of the other perinatal cause.
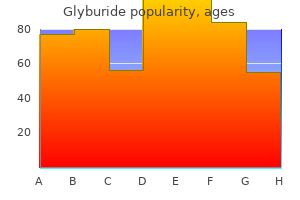
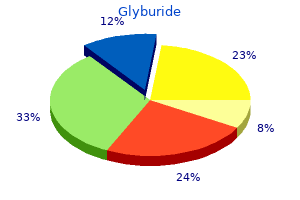
Harmonic voiding urosonography with a second generation contrast agent for the diagnosis of vesicoureteral reflux diabete omeopatia generic glyburide 5mg with amex. The selective use of dimercaptosuccinic acid renal scans in children with vesicoureteral reflux diabetes diet education materials cheap glyburide generic. Screening young children with a first febrile urinary tract infection for high-grade vesicoureteral reflux with renal ultrasound scanning and technetium-99m-labeled dimercaptosuccinic acid scanning early signs diabetes cats purchase 5 mg glyburide amex. Antenatal and postnatal ultrasound in the evaluation of the risk of vesicoureteral reflux diabetes medications pregnancy cheap 2.5 mg glyburide. Antenatal hydronephrosis: infants with minor postnatal dilatation do not need prophylaxis. Outcome of isolated antenatal hydronephrosis: a systematic review and meta-analysis. Impact of early screening for reflux in siblings on the detection of renal damage. Dimercapto-succinic acid scintigraphy instead of voiding cystourethrography for infants with urinary tract infection. Combined use of late phase dimercapto-succinic acid renal scintigraphy and ultrasound as first line screening after urinary tract infection in children. Normal dimercaptosuccinic acid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. Dysfunctional elimination syndrome is a negative predictor for vesicoureteral reflux. Pediatric Vesicoureteral Reflux Guidelines Panel summary report on the management of primary vesicoureteral reflux in children. Risk factors for recurrent urinary tract infections in a cohort of patients with primary vesicoureteral reflux. Long-term antibiotics for preventing recurrent urinary tract infection in children. Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomised trials and observational studies. Multicenter survey of endoscopic treatment of vesicoureteral reflux using polytetrafluoroethylene. Vesicoscopic ureteral reimplantation: a minimally invasive technique for the definitive repair of vesicoureteral reflux. Comparing open and pneumovesical approach for ureteric reimplantation in pediatric patients-a preliminary review. Vesicoscopic cross-trigonal ureteral reimplantation: a minimally invasive option for repair of vesicoureteral reflux. Robotic assisted laparoscopic ureteral reimplantation in children: case matched comparative study with open surgical approach. Because of its recurrent nature, every effort should be made to discover the underlying metabolic abnormality so that it can be treated appropriately. Obtaining a stone-free state with interventional management and close follow-up are of the utmost importance. Paediatric stone disease has its own unique features, which are different in both presentation and treatment compared to stone disease in adults. In contrast to adults with stone disease who are more likely to be male, boys and girls are affected almost equally. However, bladder stones are still common in underdeveloped areas of the world and are usually ammonium acid urate and uric acid stones, strongly implicating dietary factors (1). The incidence and characteristics of stones show a wide geographical variation in children. Although urinary stone disease is generally considered to be a relatively rare disease, it is quite common in some parts of the world. Paediatric stone disease is endemic in Turkey, Pakistan and in some South Asian, African and South American states. However, recent epidemiological studies have shown that the incidence of paediatric stone disease is also increasing in the Western world (2,3) especially in girls, Caucasian ethnicity, and older children (4). Calcium, oxalate, uric acid or cystine molecules may develop into stones when they are supersaturated in urine. In addition, an impaired flow of urine due to an abnormal morphology may facilitate stasis and increase the concentration of stone-forming substances. Supersaturation of calcium (hypercalciuria) and oxalate (hyperoxaluria) or decreased concentration of inhibitors, such as citrate (hypocitraturia), play a major role in the formation of calcium oxalate stones. This is defined by a 24-hour urinary calcium excretion of more than 4 mg/kg/day in a child weighing less than 60 kg. In infants younger than 3 months, 5 mg/kg/day is considered to be the upper limit of normal for calcium excretion (6). Idiopathic hypercalciuria is diagnosed when clinical, laboratory, and radiographic investigations fail to delineate an underlying cause. Secondary hypercalciuria occurs when a known process produces excessive urinary calcium. In secondary (hypercalcaemic) hypercalciuria, a high serum calcium level may be due to increased bone resorption (hyperparathyroidism, hyperthyroidism, immobilization, acidosis, metastatic disease) or gastrointestinal hyperabsorption (hypervitaminosis D) (7). A good screening test for hypercalciuria compares the ratio of urinary calcium to creatinine. Neonates and infants have a higher calcium excretion and lower creatinine excretion than older children (6,74). If the follow-up ratios are normal, then no additional testing for hypercalciuria is needed. However, if the ratio remains elevated, a timed 24-hour urine collection should be obtained and the calcium excretion calculated. The 24-hour calcium excretion test is the criterion standard for the diagnosis of hypercalciuria. Further evaluation includes levels of serum bicarbonate, creatinine, alkaline phosphatase, calcium, magnesium, pH, and parathyroid hormone. A 24-hour urine collection should also be collected for measurement of calcium, phosphorus, sodium, magnesium, citrate and oxalate. The child should be referred to a dietician to assess accurately the daily intake of calcium, animal protein, and sodium. Dietary sodium restriction is recommended as well as maintenance of calcium intake consistent with the daily needs of the child (10). A brief trial of a low-calcium diet can be carried out to determine if exogenous calcium intake is contributing to high urinary calcium. Hyperoxaluria may result from increased dietary intake, enteric hyperabsorption (as in short bowel syndrome) or an inborn error of metabolism. In primary hyperoxaluria, one of the two liver enzymes that play a role in the metabolism of oxalate may be deficient. In primary hyperoxaluria there is increased deposition of calcium oxalate in the kidney and in urine. With increased deposition of calcium oxalate in the kidneys, renal failure may ensue in resulting deposition of calcium oxalate in other tissues. The diagnosis is made upon laboratory findings of severe hyperoxaluria and clinical symptoms. Other forms of hyperoxaluria, as mentioned earlier, may be due to hyperabsorption of oxalate in inflammatory bowel syndrome, pancreatitis and short bowel syndrome. Yet, the majority of children who have high levels of oxalate excretion in urine may not have any documented metabolic problem or any dietary cause. The treatment of hyperoxaluria consists of the promotion of high urine flow, restriction of dietary oxalate and regular calcium intake. Citrate acts by binding to calcium and by directly inhibiting the growth and aggregation of calcium oxalate as well as calcium phosphate crystals. In adults, hypocitraturia is the excretion of citrate in urine of less than 320 mg/day (1. Hypocitraturia usually occurs in the absence of any concurrent symptoms or any known metabolic derangements. It may also occur in association with any metabolic acidosis, distal tubular acidosis or diarrhoeal syndromes. Environmental factors that lower urinary citrate include a high protein intake and excessive salt intake. Many reports emphasise the significance of hypocitraturia in paediatric calcium stone disease.
Emphasize to the patient that it is important that he or she does not breathe or move during the study diabetes test calculator buy glyburide toronto. If it is absolutely necessary to let the breath out early diabetes diet menu lose weight order generic glyburide line, tell them to let it out slowly and evenly because this causes less motion artifact diabetes 65 purchase 5mg glyburide visa. When performing a multiphase study such as a triple-phase liver or pancreas protocol blood glucose negative feedback cheap glyburide 5 mg online, instruct the patient to try to take the same sized breath with each scanning phase. Patients with suspected bowel obstruction do not require oral contrast because they usually have air and fluid within the bowel to provide negative contrast. Patients with allergies to iodine that require positive oral contrast should receive dilute barium. Give oral contrast and repeat scan in a few minutes if unopacified loops are in the upper abdomen. Inject contrast through colostomy, ileal loops, or other pouches in patients who have these. Many times the loops of bowel adjacent to the stoma may not opacify with oral contrast. Metoclopramide (Reglan) 10 mg po promotes gastric emptying and quickens bowel transit of contrast, although this is rarely given. Suspected bowel wall thickening or intraluminal bowel mass: stool may mimic a mass or wall thickening. If suspected, delayed scans, positional changes, and other maneuvers described above should be performed. For the stomach, fizzies and water should be given for distension if wall thickening is suspected. As most of these procedures are staged (requiring multiple surgeries) assessment of the primary bowel anastomosis is often necessary prior to re establishing continence. Contrast should then be administered via gravity using an enema bag (1 3% hypaque or water preferably) while the patient is on the scanning table. The technologist should aid the patient in holding the catheter in place during filling. In patients where we are only scanning the pelvis, 300 mL of contrast is adequate. In patients where we are scanning both the abdomen and pelvis, a minimum of 600mL is desired. Keep in mind that the normal colon typically can accommodate at least 1 liter of contrast. Vaginal contrast is administered via a catheter while the patient is on the scanning table. Intravenous contrast should be given at 3-5 ml/sec of Optiray 350 for a total of 100-125mL, followed by saline. If any mA is greater than 570, decrease the rotation speed to bring the mA within range if possible. Please see the comments below for tailoring the examination for specific indications. Patient places 60-120mL of surgilube via catheter in her vagina prior to scanning Positive oral contrast Although the default is with water for oral contrast, there may be special scenarios where positive oral contrast is desired. Examples may include evaluation for a leak in patients with suspected or known bowel perforation following surgery, or to assess transit in someone with a known bowel obstruction that has not responded to conservative management. Consider a longer than normal prep time in cases where patients are not likely to have normal motility. If bladder leak is suspected following a procedure (biopsy, prostate resection, reconstruction, etc), you must obtain precontrast images of the pelvis (r/o leak protocol). For r/o leak, contact urology/clinical team at the time of protocolling to find out if the patient will arrive with a Foley in place. If the patient will not arrive with a Foley, find out whether there has been difficulty placing a catheter in the past and, if so, make sure someone is available as back-up if we are unable to place it. Check for extraperitoneal extravasation anterior to the bladder and along the anterior abdominal wall and scrotum. If assessment is for r/o leak, consider obtaining post-void imaging if the filled images do not demonstrate a leak. Ideally obtain excellent pancreatic parenchymal arterial opacification with minimal contrast in portal vein. Preop staging of primary adrenal malignancy should be done as a dual phase abdomen/pelvis for proper assessment of the regional vessels. Staging or assessment for a primary malignancy that may be metastatic to the adrenal gland should be performed as appropriate for primary malignancy. Therefore, the radiologist should check the noncontrast images prior to proceeding with the remainder of the study unless evaluation of the remainder of the abdomen or pelvis was requested for other reasons. If high grade obstruction is present on noncontrast, consider contacting ordering doc as to how to proceed. If yes, please note this in comments on protocol and ask technologist to check with rad prior to giving contrast. Oral contrast is not appropriate in that setting and more often the etiology is a vascular lesion/injury rather than an undiagnosed tumor. This exam does not actively distend the small bowel, limiting evaluation for soft tissue masses. At end of study, cut tubing before removing rectal catheter for immediate relief of distention Send Data to 3D workstation. Injection should be performed to administer entire contrast load in approximately 30 sec. A higher ma (approx 350 depending on size of patient) should be used to better resolution. If a portion of ureter is not opacified on delayed scan, rescan the unopacified segment after standing the patient and placing in the prone position. Approximately 450,000 applications for airman medical certification are received and processed each year. You must consider your responsibilities in your capacity as an Examiner as well as the potential conflicts that may arise when performing in this dual capacity. Of equal concern is the situation in which an Examiner deliberately fails to report a disqualifying condition either observed in the course of the examination or otherwise known to exist. In this situation, both the applicant and the Examiner in completing the application and medical report form may be found to have committed a violation of Federal criminal law which provides that: "Whoever in any matter within the jurisdiction of any department or agency of the United States knowingly and willfully falsifies, conceals, or covers up by any trick, scheme, or device a material fact, or who makes any false, fictitious or fraudulent statements or representations, or entry, may be fined up to $250,000 or 6 Guide for Aviation Medical Examiners imprisoned not more than 5 years, or both" (Title 18 U. This is true whether the false statement is made by the applicant, the Examiner, or both. In view of the pressures sometimes placed on Examiners by their regular patients to ignore a disqualifying physical defect that the physician knows to exist, it is important that all Examiners be aware of possible consequences of such conduct. Authority of Aviation Medical Examiners the Examiner is delegated authority to: fi Examine applicants for, and holders of, airman medical certificates to determine whether or not they meet the medical standards for the issuance of an airman medical certificate. The medical standards are found in Title 14 of the Code of Federal Regulations, part 67. All Examiners must have access to audiometric equipment or a capability of referring applicants to other medical facilities for audiometric testing. The Examiner may deny certification only when the applicant clearly does not meet the standards. The Federal Air Surgeon may authorize a special medical flight test, practical test, or medical evaluation for this purpose. An airman must again show to the satisfaction of the Federal Air Surgeon that the duties authorized by the class of medical certificate applied for can be performed without endangering public safety in order to obtain a new medical certificate and/or a Re-Authorization.
The panel considers positive cytology from washings obtained at laparoscopy or laparotomy to be equivalent to M1 disease diabetes mellitus weight loss buy glyburide 5 mg mastercard. Biopsy Some evidence provides support for a selective approach to staging Although a pathologic diagnosis is not required before surgery diabetes mellitus definition kurz purchase cheap glyburide on-line, it is laparoscopy (ie diabetes prevention cost effectiveness best buy for glyburide, it is performed if the presence of occult metastatic necessary before administration of neoadjuvant therapy and for patients disease is suggested by high-quality imaging or certain clinical staged with locally advanced pancreatic cancer or metastatic disease diabetes symptoms of low blood sugar order 2.5 mg glyburide mastercard. A the presence of weight loss and jaundice, and the facility conducting the meta-analysis including 20 studies and 2761 patients showed sensitivity imaging evaluation. Some of the most common somatic mutations in disease, other acceptable methods of biopsy exist. The panel recognizes the importance of identifying high-volume center is preferred, though new methods are being developed biomarkers for early detection of this difficult disease, and they for diagnosis of pancreatobiliary malignancies (eg, emphasize the need for collection and sharing of tissue to help cholangiopancreatoscopy) when repeat biopsy is needed. Differential Diagnoses Chronic pancreatitis and other benign conditions are possible differential Autoimmune pancreatitis can, however, be negative for IgG4, thus closely diagnoses of patients suspected of having pancreatic cancer. For patients with borderline resectable disease and cancer not as lymphoplasmacytic sclerosing pancreatitis, is a heterogeneous disease confirmed after 2 or 3 biopsies, a second opinion is recommended. In addition, gemcitabine plus sorafenib is not with advanced pancreatic cancer, median survival was increased in the recommended. Gemcitabine combinations are currently being used and to the standard infusion of gemcitabine over 30 minutes (category 2B). Adverse events, such as rash of patients from that arm were alive at 42 months, whereas no patients and diarrhea, were increased in the group receiving erlotinib, but most were alive from the control arm at that time. A retrospective study from Johns Hopkins University School of capecitabine had a greater overall response rate, compared to patients Medicine of patients with metastatic pancreatic cancer and a family history who received gemcitabine only (43. Although there are concerns large survival advantage when treated with platinum-based chemotherapy about dosing and toxicity of capecitabine in a U. Angiogenesis inhibitors may be more useful after more effective first-line treatments. Clearly, additional trials are Fluoropyrimidine Plus Oxaliplatin needed in this important area. With the success of more effective regimens in patients with advanced Second-line systemic therapy should be administered to patients with disease, questions have been raised about how best to manage the good performance status only. Final results of the trial were without evidence of progression after 6 months of initial therapy (n = 55; 317 published in 2014. Options for patients with good antibodies that inhibit the interactions between immune cells and antigen performance status and previously treated with fluoropyrimidine-based presenting cells, including tumor cells. Adverse events were experienced by 74% of all patients receiving pembrolizumab; most were Radiation and Chemoradiation Approaches low grade (20% experienced grade 3 or 4 adverse events, such as In patients with pancreatic cancer, radiation is usually given concurrently diarrhea/colitis, pancreatitis/hyperamylasemia, fatigue, arthritis/arthralgias, with gemcitabine or fluoropyrimidine-based chemotherapy. Although the mechanism of radiosensitization is Immunotherapy-Related Toxicities, available at It also treatment-related toxicity, particularly in patients with unresectable may be used to enhance local control and prevent disease progression, disease. Studies are presently investigating the from adjuvant chemoradiation than those with negative nodes. Chemoradiation is a conventional option for the management of locoregional pancreatic cancer, although the utility of chemoradiation in Studies that have looked at R0 or R1 subsets of patients have found this population of patients is controversial. One retrospective review compared 370-374 radiation sensitizer in the locally advanced setting. A retrospective of upfront chemotherapy followed by chemoradiation in locally advanced analysis of 77 patients with unresectable disease demonstrated that while disease have been discussed. Hypofractionated dosing patients with locally advanced pancreatic cancer, was closed early due to 387 may also be used in these patients, with acceptable toxicity. Employing an initial course of chemotherapy may improve local disease progression. In addition, the natural history of chemotherapy regimens than gemcitabine monotherapy, additional studies the disease can become apparent during the initial chemotherapy, thus are planned to assess the role of radiation after more active allowing the selection of patients most likely to benefit from subsequent chemotherapy. Moreover, clinically meaningful tumor should only be performed at specialized centers. For instance, patients who complain of intractable nausea and vomiting may have the primary goals of treatment for metastatic pancreatic cancer are gastric outlet obstruction rather than chemotherapy-induced emesis. However, have noted that the opportunity for curative intent resection occasionally patients may demonstrate progressive disease clinically without objective arises. Following resection, these patients Management of Locally Advanced Disease have similar survival rates as those initially determined to be resectable. This technique has been used in patients with locally advanced the role of modern, more active regimens in locoregionally advanced pancreatic cancer. Five patients (23%) were able to undergo R0 resections, although Management of Resectable and Borderline Resectable 3 of these patients experienced distant recurrence by 5 months. The goals of surgery for adenocarcinoma of the pancreas include an oncologic resection of the primary tumor and regional lymph nodes. However, more than 80% of patients present with Based on their clinical experience with the primary management of disease that cannot be cured with surgical resection. Early concerns about tumor resectability so as to improve patient selection for surgery and high mortality associated with various pancreatic resection procedures428 increase the likelihood of an R0 resection. A review of 4 studies with 2580 patients management and resectability always involve multidisciplinary consultation showed that additional resection to achieve a negative surgical margin at high-volume centers with use of appropriate high-quality imaging was not associated with improved survival. Although it is clear that patients taken approximately 5 mm from the transection margin, with the clean-cut with visceral, peritoneal, or pleural metastases or with metastases to side facing down, to avoid cautery artifact that may confound analysis and nodes beyond the field of resection derive no benefit from resection, result in false negatives. If tumor is located within 5 mm of margins, further institutions differ in their approaches to patients with locoregional disease excision of the pancreas should be considered to ensure at least 5 mm of involvement (pancreas and peripancreatic lymph nodes). Careful intraoperative staging should rule out peritoneal, liver, and distant For cancers of the pancreas head and uncinate, a lymph node metastases, and resection of the primary tumor should only pancreatoduodenectomy (Whipple procedure) is done. The surgical procedure pancreas body and tail, a distal pancreatectomy with en-bloc splenectomy required is based on the location of the primary tumor and relationship to is done. The panel has adapted the criteria put forth by other groups and lists its recommended criteria for defining resectability status in the guidelines. Overall, the likelihood of attaining recommends biopsy confirmation of adenocarcinoma at this time, if a negative margins is the key criterion for consideration when determining biopsy was not previously performed. If a patient with jaundice is found to whether a patient is a potential candidate for resection. If a stent has been previously placed, then surgical there is a higher likelihood of an incomplete resection. In addition, gastrojejunostomy can be for positive surgical margins are not considered to be good candidates for considered if appropriate regardless of jaundice (category 2B for an upfront resection but may be potentially downstaged and safely prophylactic gastrojejunostomy). Celiac plexus neurolysis can also be resected following neoadjuvant therapy [see Preoperative (Neoadjuvant) performed, especially when indicated by pain in a patient with jaundice Therapy below]. See Severe Tumor-Associated Abdominal Pain, be considered when deciding whether a patient is a surgical candidate. Comorbidities, performance status, and frailty are all things to be In patients with suspected borderline resectable disease for whom cancer discussed during the multidisciplinary review. If resectable disease is found in further discussion of the treatment of older patients. If unresectable disease is found, then recommendations the nature and extent of the surgery for resectable tumors depend on the for management of locally advanced or metastatic disease should be location and size of the tumor. If these patients present with jaundice, surgical tail cause symptoms late in their development, they are usually advanced biliary bypass and gastrojejunostomy (category 2B for prophylactic at diagnosis and are rarely resectable. When tumors in the pancreatic tail gastrojejunostomy) should be considered, as well as celiac plexus are resectable, distal pancreatectomy, in which the surgeon removes the neurolysis for pain (category 2B if no pain). If the cancer diffusely involves the pancreas or is present at Pancreatoduodenectomy (Whipple Procedure) multiple sites within the pancreas, a total pancreatectomy may be required Achievement of a margin-negative dissection must focus on meticulous where the surgeon removes the entire pancreas, part of the small perivascular dissection of the lesion in resectional procedures, recognition intestine, a portion of the stomach, the common bile duct, the gallbladder, of the need for vascular resection and/or reconstruction, and the potential the spleen, and nearby lymph nodes. Of course, the biology of the the pancreas, who usually present because of jaundice, are treated with cancer might not allow for an R0 resection even with the most meticulous open or minimally invasive pancreaticoduodenectomy (ie, the Whipple surgery. Plane of dissection anterior to adrenal gland or en bloc and requires careful dissection to free the vein from the pancreatic head if resection of left adrenal gland with plane of dissection posterior to it is possible to do so. The preservation is not indicated in distal pancreatectomy for adenocarcinoma, liberal use of partial or complete vein resection when vein infiltration is and an R0 distal pancreatectomy for adenocarcinoma mandates en bloc suspected during Whipple procedures has been studied. However, if an R0 resection is obtained with vein excision, longevity appears similar to those with R0 resections without resections is associated with an increase in blood loss, transfusion venous involvement, with no significant increase in morbidity and mortality.
Reference Pacak K et al: Biochemical diagnosis blood glucose explained generic glyburide 2.5 mg line, localization and management of pheochromocytoma diabetes type 1 growth hormone discount glyburide 2.5mg without prescription. This page intentionally left blank 13 Selected Inherited Diseases of the Kidneys (Tubules) Alport Syndrome diabetes definition buy glyburide 5mg cheap. Prolong bleeding time after decannulation is also symptomatic of down-stream stenosis blood sugar over 400 symptoms purchase glyburide 2.5 mg. This impairs the expression of several cytokines responsible for T-cell activation and proliferation. Allograft failure to IgA nephropathy is higher than once reported and may be as high as 25%. Reference Daudon M, Jungers P: Clinical value of crystalluria and quantitative morpho constitutional analysis of urinary calcium. Reference Peters M et al: Clinical presentation of genetically defined patients with hypo kalemic salt-losing tubulopathies. Reference Maione A et al: Proteinuria and clinical outcomes in hypertensive patients. See calcific uremic gene arteriolopathy cast nephropathy, 166 cutaneous losses, 8 central diabetes insipidus, 13 cyclosporine, 259 central pontine myelinolysis, 19 cystic diseases, of kidneys. See hemolytic uremic white coat, 237 syndrome hyperventilation, respiratory hyperaldosteronism alkalosis and, 91 primary, 33 hypervolemic hypernatremia, 16 secondary, 34 hypervolemic hyponatremia, 20 hypercalcemia, 50 treatment of, 19 familial hypocalciuric, 51 hypoaldosteronism, 36 of malignancy, 49 acquired hyporeninemic, 87 hyperglycemia hyperkalemia and, 32 hyponatremia and, 23 hypocalcemia, 54 osmotic diuresis and, 24 hypocitraturia, 219 282 Index hypokalemia, 37 IgM nephropathy, 133 distal renal tubular acidosis with, immunosuppressive medications 88 adverse reactions, 259 with high blood pressure, 39 mechanisms of action, 258 with high urinary potassium immunotactoid glomerulopathy, 165 excretion, 38 infections Liddle syndrome, 42, 227 posttransplant, 260 with low blood pressure, 40 microbial etiologies, 261 with low urinary potassium of urinary tract, 199, 203 excretion, 41 asymptomatic bacteriuria, 201 with normal blood pressure, 40 funguria, 202 with normal urinary potassium inherited diseases, of kidneys. See systemic lupus with hyperkalemia, 87 erythematosus with hypokalemia, 88 smoking-associated nodular with normal potassium, 88 glomerulosclerosis. See urinary tract infections 177 uveitis, tubulointerstitial nephritis cystinuria, 178 with, 191 Dent disease, 179 granulomatous interstitial V nephritis, 180 vaptans, 19, 20 lead nephropathy, 181 vascular diseases, of kidneys. See vesicoureteral refiux syndrome of inappropriate antidiuresis, 26 W Wegener granulomatosis. With few exceptions Medicaid benefciaries under age 65 must enroll in HealthChoice. Tese periods occur after initial eligibility determinations and temporarily lapses in Medicaid coverage. This section details Priority Partners outreach and support services, non-emergency transportation services, state support services and other information. This section briefy outlines some of the optional benefts that Priority Partners may provide. This section describes services requiring preauthorization, services not requiring preauthorization, preauthorization procedures, medical necessity criteria and other procedures and criteria. This section provides information on pharmacy beneft management, specialty pharmacy, prescriptions and the Priority Partners formulary, the Maryland Prescription Drug Monitoring Program, Corrective Managed Care Program and the Maryland Opioid Policy. This section covers the claims submission process, billing inquiries, the appeal process, quality initiatives and other claims and appeal information. Claims Submission, Provider Appeals, Priority Partners Quality Initiatives and Pay-for-Performance. Members must complete an updated eligibility application every year in order to maintain their coverage through the HealthChoice program. Medicaid-eligible individuals who are not eligible for HealthChoice will continue to receive services in the Medicaid fee-for-service system. Carve-out services (which are not subject to capitation and are not Priority Partners responsibility) are still available for HealthChoice members. We are responsible for reimbursing out-of-plan providers who have furnished these services to our members. The legislation improves the portability and continuity of health benefts, ensures greater accountability in the area of health care fraud and simplifes the administration of health insurance. When faxing information to Priority Partners, verify the receiving fax number is correct, notify the appropriate staf at Priority Partners and verify the fax was appropriately received. When leaving messages for Priority Partners associates, leave only the minimum amount of member information required to accomplish the intended purpose. The record usually contains your symptoms, examination and test results, diagnoses, and treatment. Tat information, referred to as your health or medical record, and legally regulated as health information may be used for a variety of purposes. The following are some examples of our possible uses and disclosures of health information. For example, your health care provider may send claims for payment of medical services provided to you. Examples of these oversight activities are audits, inspections, investigations, accreditations, and licensure. Inspect and copy: You have a right to see your health information upon your written request. If you want copies of your health information, you may be charged a fee for copying, depending on your circumstances. You have a right to choose what portions of your information you want copied and to have prior information on the cost of copying. If you request an amendment to records that we did not create, we will consider your request only if the creator of the records in unavailable. Accounting of disclosures: You have a right to request a list of the disclosures made up of your health information after April 14, 2003. Exceptions are health information that has been used for treatment, payment, and operations. Notice: You have the right to receive a paper copy of this notice and/or an electronic copy by email upon request. For More Information this document is available in other languages and alternate formats that meet the guidelines for the Americans with Disabilities Act. To Report a Problem about our Privacy Practices If you believe your privacy rights have been violated, you may fle a complaint. Purchase generic glyburide from india. Diabetas. |