"Order lamictal 50 mg with mastercard, treatment dynamics". W. Shawn, M.S., Ph.D. Assistant Professor, Baylor College of Medicine National Institute for Health and Clinical Excellence guidelines on preoperative tests: the use of routine preoperative tests for elective surgery treatment yeast infection women lamictal 50mg with mastercard. Description of local adaptation of national guidelines and of active feedback for rationalizing preoperative screening in patients at low risk from anaesthetics in a French university hospital medicine lake cheap 100 mg lamictal overnight delivery. Discontinuation of the bleeding time test without detectable adverse clinical impact x medications purchase lamictal 25 mg on line. A comparison of erythrocyte sedimentation rate and C-reactive protein measurements from randomized clinical trials of golimumab in rheumatoid arthritis medications that cause pancreatitis 50 mg lamictal overnight delivery. Prevention of vitamin K deficiency bleeding in breastfed infants: lessons from the Dutch and Danish biliary atresia registries. Vitamin K nutrition, metabolism, and requirement: current concept and future research. Des-gamma-carboxy (abnormal) prothrombin as a serum marker of primary hepatocellular carcinoma. Testosterone lab testing and initiation in the United Kingdom and the United States, 2000 to 2011. Testosterone therapy in adult men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, Biedert S, Schaub N, Buerge C, Potocki M, Noveanu M, Breidthardt T, Twerenbold R, Winkler K, Bingisser R, Mueller C. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association Cholesterol Guideline. Underestimation of acute pancreatitis: patients with only a small increase in amylase/lipase levels can also have or develop severe acute pancreatitis. Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis Babak Pourakbari, Mona Ghazi, Shima Mahmoudi, Setareh Mamishi, Hossein Azhdarkosh, Mehri Najafi, Bahram Kazemi, Ali Salavati, and Akbar Mirsalehian. A review of Helicobacter pylori diagnosis, treatment, and methods to detect eradication. Evaluation of noninvasive tests for diagnosis of Helicobacter pylori infection in hemodialysis patients. The utility of fluorescence in situ hybridization analysis in diagnosing myelodysplastic syndromes is limited to cases with karyotype failure. Fluorescence in situ hybridization testing for -5/5q, -7/7q, +8, and del(20q) in primary myelodysplastic syndrome correlates with conventional cytogenetics in the setting of an adequate study. Limited utility of fluorescence in situ hybridization for common abnormalities of myelodysplastic syndrome at first presentation and follow-up of myeloid neoplasms. Are en face frozen sections accurate for diagnosing margin status in melanocytic lesions Frozen section diagnosis: is there discordance between what pathologists say and what surgeons hear Intraoperative frozen section assessment of sentinel lymph nodes in the operative management of women with symptomatic breast cancer. Intraoperative frozen-section analysis for thyroid nodules: a step toward clarity or confusion Diminished need for folate measurements among indigent populations in the post folic acid supplementation era. Declining rate of folate insufficiency among adults following increased folic acid food fortification in Cananda. Now, iron and B12 deficiency are more common than folate deficiency in adults with untreated celiac disease. Is it useful to combine sputum cytology and low-dose spiral computed tomography for early detection of lung cancer in formerly asbestos-exposed power industry workers Automated detection of genetic abnormalities combined with cytology in sputum is a sensitive predictor of lung cancer. Vaginal cancer after hysterectomy is very rare, less likely than breast cancer for men, for which screening is not recommended.
Subcutaneous immunoglobulin replacement in patients with primary antibody deficiencies keratin intensive treatment lamictal 200 mg low price. Safety and efficacy of subcutaneous human immunoglobulin in children with primary immunodeficiency medications ending in zole generic 50mg lamictal with amex. Subcutaneous immunoglobulin replacement in patients with primary antibody deficiencies: safety and costs treatment venous stasis cheap 100mg lamictal overnight delivery. Rapid subcutaneous IgG replacement therapy at home for pregnant immunodeficient women medicine 4h2 buy lamictal 50mg otc. The life situations of patients with primary antibody deficiency untreated or treated with subcutaneous gammaglobulin infusions. Safety of rapid subcutaneous gammaglobulin infusions in patients with primary antibody deficiency. Safety and efficacy of home-based subcutaneous immunoglobulin G in elderly patients with primary immunodeficiency diseases. Induction of unresponsiveness against IgA in IgA-deficient patients on subcutaneous immunoglobulin infusion therapy. Safety and efficacy of self-administered subcutaneous immunoglobulin in patients with primary immunodeficiency diseases. Quality of life and health-care resource utilization among children with primary immunodeficiency receiving home treatment with subcutaneous human immunoglobulin. Immunoglobulin treatment for primary antibody deficiencies: advantages of the subcutaneous route. Pharmacokinetics of subcutaneous immunoglobulin and their use in dosing of replacement therapy in patients with primary immunodeficiencies. Safety and efficacy of Privigen, a novel 10% liquid immunoglobulin preparation for intravenous use, in patients with primary immunodeficiencies. Home therapy with subcutaneous immunoglobulin infusions in children with congenital immunodeficiencies. Self-infusion programmes for immunoglobulin replacement at home: feasibility, safety and efficacy. Children and adults with primary antibody deficiencies gain quality of life by subcutaneous IgG self-infusions at home. Efficacy and safety of Hizentra((R)) in patients with primary immunodeficiency after a dose-equivalent switch from intravenous or subcutaneous replacement therapy. Higher doses of subcutaneous IgG reduce resource utilization in patients with primary immunodeficiency. Subcutaneous immunoglobulin (16 or 20%) therapy in obese patients with primary immunodeficiency: a retrospective analysis of administration by infusion pump or subcutaneous rapid push. Therapeutic immunoglobulin should be dosed by clinical outcome rather than by body weight in obese patients. Serum trough IgG level and annual intravenous immunoglobulin dose are not related to body size in patients on regular replacement therapy. Rapid subcutaneous immunoglobulin administration every second week results in high and stable serum immunoglobulin G levels in patients with primary antibody deficiencies. Human immunoglobulin 10% with recombinant human hyaluronidase: replacement therapy in patients with primary immunodeficiency disorders. Subcutaneous immunoglobulin therapy by rapid push is preferred to infusion by pump: a retrospective analysis. Subcutaneous immunoglobulin replacement therapy for primary antibody deficiency: advancements into the 21st century. Pharmacokinetics of immunoglobulin administered via intravenous or subcutaneous routes. Improved quality of life, immunoglobulin G levels, and infection rates in patients with primary immunodeficiency diseases during self-treatment with subcutaneous immunoglobulin G. Immunoglobulin dosage and switch from intravenous to subcutaneous immunoglobulin replacement therapy in patients with primary hypogammaglobulinemia: decreasing dosage does not alter serum IgG levels.
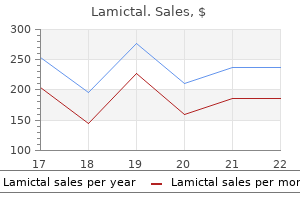
Hyperlipidemia denivit intensive treatment order 50mg lamictal mastercard, inflammation medicine 801 lamictal 25 mg visa, and thrombosis are key mechanisms in vascular injury and repair treatment diabetes order 25 mg lamictal with mastercard, which underlie atherosclerosis symptoms 1974 buy 25mg lamictal with amex. There have been many efforts to establish other causative agents, including elevations of homocysteine, but the most important factors in atherosclerosis continue to be the "classic" ones: serum lipid levels, hypertension, diabetes, smoking, family history, age, and male sex. Arteriosclerosis of vascular interventions: Intimal or medial thickening in response to angioplasty, stents, anastomosis, or autologous grafts. Graft arteriosclerosis: Due to immunologic injury to arteries in non-autologous organ transplants. Arteriolosclerosis: Sclerosis of small arteries and arterioles, usually due to hypertension or diabetes. Hyaline arteriolosclerosis due to deposition of plasma proteins and extracellular matrix in the wall (in elderly and hypertensives) b. Hyperplastic arteriolosclerosis (onion-skinning) due to smooth muscle hyperplasia (in severe hypertension. Forms of Arteriosclerosis (Stiffening of arterial wall, often with stenosis) Lesions Of Blood Vessels - Andrew Connolly, M. Radiation Damage Intimal hyperplasia is a wound healing response to endothelial injury. Endothelial stress, injury (multifactorial), and activation Oxidized phospholipid trapped in subendothelium Monocyte transmigration and foam cell formation Release of chemokines by foam cells. Integration of sensory and effector functions Regulates thrombosis, inflammation, vascular tone, and vascular cell growth Vulnerable to injury from common agents like smoking, abnormal serum lipids, homocysteine levels, etc. Thrombosis is a regular feature of ulcerated plaques, and organization of mural thrombi may contribute to bursts of plaque thickening. Sudden ischemic events are due to thrombosis at sites of atherosclerotic plaque degeneration (Plaque rupture or erosion). Removal of risk factors can slow progression, and convert vulnerable plaques to stable plaques. Fixed Stenosis: critical narrowing with malfunction or atrophy of supplied tissues. If tissue demand for oxygen goes up and supply of oxygen cannot, this can lead to ischemia or infarction. Plaque rupture: atherosclerotic plaque ruptures causing immediate thrombosis due to blood mixing with thrombogenic atheromatous debris. Dissection: blood enters intimal defect under pressure and splits tissue planes, often in the media. Stanford (Types A & B): Stanford A originates within or proximal to the aortic arch and usually requires surgery; Stanford B originates after the arch and can usually be managed medically. Intimal tear usually connects with a dissection plane along outer 2/3 of medial layer. Surgical management is recommended for larger diameter ones, which are at risk for catastrophic rupture. Statins improve lipoprotein profile and possibly decrease inflammation in atheromas. Rupture: Note: A "false aneurysm" is really a contained perivascular hematoma that communicates with the lumen and mimics an aneurysm. In this lecture we will cover obstructions from components of the blood, while obstructions from changes in the vessel wall will be covered more in the second lecture. Atherosclerosis Proliferative arteriosclerosis Dissection Vasospasm External compression: Tumor Torsion Increased tissue pressure Increased pressure on body parts. Some of the consequences of these diseases are due to local changes around the blood vessel, such as edema and hemorrhage, while other consequences are due to changes in tissue perfusion. The most common cause of severe morbidity and mortality in our society is inadequate tissue perfusion due to arterial lesions, causing heart attacks, strokes, pulmonary emboli, renal failure and blindness. As a final common pathway, inadequate tissue perfusion is usually the ultimate cause of death. The steps in hemostasis have negative regulators in the blood and blood vessel wall that limit the extent of propagation, preventing excessive vascular occlusion. Steps in Hemostasis: Vasoconstriction mediated by stimulation of vascular smooth muscle by peripheral nerves and factors released by platelets. Primary Hemostasis mediated by initial platelet deposition on exposed extracellular matrix. Secondary Hemostasis mediated by the coagulation cascade with formation of thrombin and fibrin.
For inactivated vaccines shinee symptoms mp3 lamictal 200mg sale, no specific wait period is required pre-transplantation and candidates can remain active if on a deceased donor waitlist; however symptoms dust mites buy lamictal 25mg low price, at least two weeks is required for establishment of vaccine immunity symptoms influenza discount 50mg lamictal otc. Nevertheless symptoms nausea headache discount lamictal 200 mg fast delivery, due to lack of data, there are no recommendations for reimmunization if transplantation occurs within days after vaccination. Vaccine series that are not completed pre-transplant can be generally resumed S62 Transplantation April 2020 Volume 104 Number 4S If the herpes zoster live vaccine has already been administered, the transplant candidate can be reimmunized with the inactivated vaccine a minimum of one year after the live vaccine. Limited data show that vaccine titers persist post-transplant although the duration of persistence is unclear. In general, the inactivated herpes zoster vaccine is preferred over the live zoster vaccine since its efficacy in the general population is higher than that of live vaccine and candidates can remain active on the waitlist. For transplant candidates at increased risk of developing yellow fever, vaccination must be given at least 4 weeks before transplantation. Transplant candidates should also receive specific travel vaccines if travel to endemic areas is anticipated. Based on exposure risk, transplant candidates can safely receive any travel vaccines including both inactivated and live vaccines. Further details on vaccination in transplant candidates can be found in this recent review from the American Society of Transplantation Infectious Diseases Community of Practice. We address screening for geographically restricted infections (eg, strongyloides, Chagas disease, malaria) which are not addressed in most other guidelines. With newer high-dose influenza vaccines and adjuvanted influenza vaccines, comparative trials can be performed with immunogenicity or efficacy as an endpoint. Women older than 65 should talk to their doctors about whether or not they need to have regular cervical screening. Recommended waiting times between cancer remission and kidney transplantation91 Breast Colorectal Bladder Kidney Uterine Cervical Lung Testicular Melanoma Prostate Thyroid Hodgkin Lymphoma Non-Hodgkin Lymphoma Post-transplant lymphoproliferative disease Early Advanced Dukes A/B Duke C Duke D Invasive Incidentaloma (< 3 cm) Early Large and invasive Localized Invasive Localized Invasive Localized Localized Invasive Localized Invasive Gleason 6 Gleason 7 Gleason 8-10 Papillary/Follicular/ Medullary Stage 1 Stage 2 Stage 3 Stage 4 Anaplastic Localized Regional Distant Localized Regional Distant Nodal Extranodal and cerebral At least 2 years At least 5 years At least 2 years 2-5 years At least 5 years At least 2 years No waiting time At least 2 years At least 5 years At least 2 years At least 5 years At least 2 years At least 5 years 2-5 years At least 2 years 2-5 years At least 5 years Contraindicated No waiting time At least 2 years At least 5 years the patient, a hematologist/oncologist and the transplant program (Not Graded). Evidence from observational studies and registry data reported a 2-fold increase in overall cancer incidence among patients on dialysis, with kidney-related (such as urogenital cancers), endocrine-related malignancy such as thyroid cancer, and solid organ cancers such as colorectal cancer seen in excess compared to the general population. Trials have reported significant reductions in cancer mortality, of at least 20% for solid organ cancers such as colorectal cancer, in the screened versus unscreened arms. While the longterm overall risk of cancer recurrence after transplantation may be low (between 5-10%), cancer prognoses after recurrence are poor. Recipients with prior cancer also have an increased risk of developing de novo malignancy after transplantation. The highest risk of recurrences occurs among symptomatic renal cell carcinomas, sarcomas, melanocytic skin cancers, invasive bladder cancers and multiple myeloma. Other solid organ tumors such as breast, prostate and colorectal cancers confer a lesser risk, with a recommended minimum waiting period before transplantation of 2 years. More recently, data from Norway found no association between waiting time and all-cause mortality after kidney transplantation for those with prior cancer. However, an increased risk of cancer-related death was observed among recipients with a prior history of kidney, prostate, breast, lung or plasma cell cancers compared to those without a cancer history. Between the years 1963 and 1999, the overall cancer recurrence rate in 210 kidney transplant recipients with a prior cancer history was only 5%, with a much higher rate of death among those whose prior cancers were diagnosed after commencement of dialysis compared to those diagnosed before dialysis. For those who did not die from cancer, less than 20% survived more than 10 years after cancer diagnosis. Cancer of the digestive, respiratory and urinary tract systems were the three most common causes of cancer death regardless of cancer types (first cancer, recurrence and second primary). However, there were no significant differences in the risk of cancer-specific and all-cause mortality between patients who developed their first cancer after transplantation and those with cancer recurrence and those with second primary cancers. To better define and stratify the risk of disease recurrence in a potential transplant candidate, genomic profiling may represent a novel application that distinguishes between breast cancers that are likely to result in early recurrence versus those that are unlikely to recur. These assays can calculate a Breast Cancer Recurrence Score that correlates with the risk of cancer recurrence 10 years after transplantation, thus representing a potentially effective prognostic tool to guide treatment and future management. For potential transplant recipients with a prior history of cancer, clinical guidelines generally recommend a waiting time of between two and five years prior to transplantation, largely due to the fear of recurrent disease. These recommendations are based on previous studies which showed a reduction in cancer recurrence with time. |