J. Eduardo Calonje, MD, DipRCPath
This result is not surprising since the liquid emptying is considered to be less sensitive than solid emptying (Christian fungus gnats bleach buy genuine lamisil line, Datz et al fungus covered chest buy cheapest lamisil and lamisil. In conclusion fungus mutant generic lamisil 250mg with visa, the reproducibility of the modified test meal for scintigraphic quantification of solid and liquid phase gastric emptying has been demonstrated fungus gnats molasses discount lamisil 250mg without prescription, provided inter-individual and intra-individual differences in gastric emptying are appreciated. The normal range data provide an initial validation for the future use of this meal in patients. Although the T50 emptying times have been used in this study it is not intended that this will be the sole criterion for determination of gastric emptying. This meal has subsequently been found to be acceptable to patients in the early postoperative phase (Chapter 6) (Lobo, Bostock et al. Gastric emptying was restored to normal either by salt and water restriction or a high protein intake. Whether these changes were due to hypoalbuminaemia, to positive sodium balance, or both is unclear. Such changes in postoperative patients, receiving crystalloid infusions, are exacerbated by their diminished ability to excrete an excess sodium and water load (Coller, Campbell et al. Several authors have described an increase in postoperative complications and adverse outcome associated with excess sodium and water administration in the perioperative period (Alsous, Khamiees et al. This study of patients was designed to test whether the phenomenon of delayed gastric emptying postoperatively described by Mecray et al. Those excluded were patients with preoperative evidence of impaired renal function, congestive cardiac failure, hepatic disease, diabetes mellitus, ascites, peritoneal metastases, or impaired mobility, along with those with significant anaemia (haemoglobin <10 g/dL) and those receiving medications affecting gastrointestinal motility. Hemicolectomy patients were selected as a model for this study only because they were a relatively homogeneous group in which to compare the effects of the two different 94 fluid regimens upon salt and water balance and gastrointestinal physiology. Patients in this group were also unlikely to require blood or colloid transfusion, or upper gastrointestinal surgical procedures which might have affected the results. Patients were randomised to one of two groups: Standard patient management (standard) group: Patients were managed on the surgical wards and received standard postoperative fluids, as practised on those wards at our hospital. This regimen contained at least 154 mmol sodium and 3 L water per day (typically, 1 L 0. Fluid prescriptions were charted independently by surgical staff and were not influenced by the investigators. Salt and water restriction (restricted) group: Patients were managed on the Clinical Nutrition Unit and normally received no more than 77 mmol sodium and 2 L water per day (typically, 0. There was an option to increase fluid input if blood urea concentrations rose or if there were clinical indications of salt or water depletion. Patients in both groups received between 40 and 60 mmol potassium per nd day from the 2 postoperative day onwards, according to the serum potassium concentration. Intraoperative fluids were prescribed by the anaesthetists involved, who were unaware of the details of the study or the randomisation. Once patients in the restricted group left the operating theatre, the investigators controlled all intravenous prescriptions, while in the standard group fluids continued to be prescribed by the anaesthetic and surgical team responsible. Clinical decisions regarding discontinuation of intravenous fluids, commencement of diet and discharge from hospital were made by the treating surgical team and not by the investigators. All patients had midline laparotomies and postoperative pain was managed by patient-controlled analgesia devices delivering morphine. Secondary end points included duration of postoperative hospital stay, and time to first passage of flatus and faeces, to discontinuation of intravenous fluids, to full mobility and to resumption of a normal diet. This gave a sample size of 20 in each group for a 0·05 difference with a power of 90%. A preliminary analysis on the first 10 patients studied showed that this difference was 74 minutes (effect size = 1·4 standard deviations), and the sample size was recalculated to be 10 in each group, so as to minimise the number of subjects in the study. All measurements on day 0 (day of operation) were made between the start of the operation and midnight. Postoperative body weight was recorded daily between 0800 and 0900 hours and blood was sampled during the same period. Intraoperative fluid and electrolyte intake and blood loss were recorded, as were daily intravenous water, sodium, potassium and oral fluid intakes, urine output and other fluid losses from days 0 to 4. Serum concentrations of sodium, potassium, urea, creatinine, and osmolality were measured daily for six days. Daily urinary sodium and potassium excretion and osmolality were measured in 97 24 h collections from days 0 to 4. Full blood count and serum albumin concentration were measured preoperatively and on postoperative days 1, 2, 4 and 6 (day 5 for those patients who were discharged on that day). Postoperative hospital stay and time to first passage of flatus and faeces, discontinuation of intravenous fluids, full mobility and resumption of a normal diet were recorded. Patients were examined daily for the presence of ankle, conjunctival or sacral oedema. Infectious and non-infectious complications and readmissions during the first 30 postoperative days were also recorded. Patients who were vomiting on the day of the gastric emptying studies, or those who had a nasogastric aspirate >1000 mL over the 24 hrs preceding the test, were assumed to have prolonged gastric emptying in accordance with previously published data (Mackie, Hulks et al. For statistical calculations, these patients were assumed to have a T50 = the longest recorded T50 + 1 min. None of the patients received any opiate or antiemetic (except those who were vomiting) during the 6 h preceding the gastric emptying studies. The assays were based upon 125 the competition between labelled I-peptide and unlabelled peptide binding to a limited quantity of specific antibody (2000; Patrono and Peskar 1987). The 125 amount of I-peptide bound as a function of the concentration of the unlabelled peptide in standard reaction mixtures (1, 2, 4, 8, 16, 32, 64 and 128 pg/mL) was measured and a standard curve constructed from which the concentration of the peptide in the unknown samples was determined. Spearman’s rank correlation was used for statistical relationships and linear regression lines were plotted on graphs. The preoperative demographic and biochemical profiles of the patients in the two groups were well matched (Table 6. No patient received blood transfusion and the total operating time was not more than 2 h in any patient. This was reflected in the higher positive cumulative sodium and water balance (Table 6. Patients in the restricted group were able to drink significantly greater quantities of fluids (Fig. Urine volume and urinary sodium and potassium excretion were not significantly different over 4 days in the two groups (Fig. None of the patients in the restricted group needed or received extra salt and water over and above the protocol regimen. The doses of morphine received by patients in the two groups from days 0-3 were almost identical (Fig. Solid lines represent medians, shaded areas interquartile ranges and whiskers extreme values. Median solid and liquid th phase gastric emptying times (T50) were significantly prolonged on the 4 postoperative day in the standard group (175 and 110 min respectively), compared to the restricted group (72·5 and 73·5 min respectively) (Fig. A linear relationship between gastric emptying time and cumulative sodium balance from days 0-4 was demonstrated (Fig. The three patients in the standard group th who were vomiting on the 4 postoperative day and unable to have gastric emptying studies done were in the greatest cumulative positive sodium balance. Patients in the restricted group fared better with regard to the secondary end points (Table 6. Whether these effects are due to fluid gain, hypoalbuminaemia or both is impossible to determine since the two are inseparable even in normal subjects in whom striking falls in serum 108 albumin concentration have been demonstrated with crystalloid infusions (Chapters 10, 11 and 12) (Lobo, Stanga et al. These results have important implications for the management of surgical patients who receive intravenous fluids. Despite the fact that postoperative patients have a diminished ability to excrete water, sodium and chloride, some centres continue to prescribe 3 L fluid and 154 mmol sodium and chloride per day even to uncomplicated postoperative patients (Chapter 7) (Lobo, Dube et al. The present study has shown that adherence to this regimen leads to a progressive accumulation of salt and water in the early postoperative period, as illustrated by the data in Table 6. By the end of day 4, after correcting for insensible losses, fluid balance was positive by 3 L in the standard group compared with zero in the restricted group. That serial weighing is the best measure of fluid balance is well known and one we have used previously in normal subjects (Chapters 10-13) (Lobo, Stanga et al.
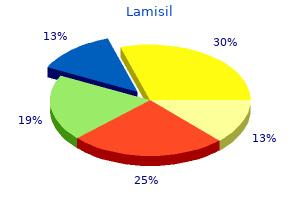
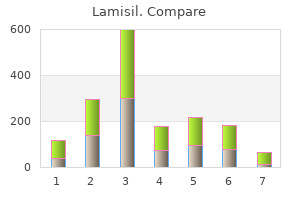
Prevalence of are some of the most commonly used medications non-steroidal anti-inflammatory drug-induced worldwide antifungal kidney damage purchase lamisil with paypal. The most common side effects are ulcers in enteropathy determined by double-balloon the digestive tract including stomach fungus gnats thrips discount 250 mg lamisil with visa, small bowel antifungal wipes for dogs buy discount lamisil 250mg on-line, endoscopy: a Japanese multicenter study antifungal wood treatment cheap 250mg lamisil amex. Non h y p o a l b u m i n e m i a, v i t a m i n B 1 2 o r b i l e a c i d steroidal anti-inflammatory drug induced injury to malabsorption, diarrhea, and acute abdominal pain. Acta Medica (Hradec Kralove) Serious complications especially massive bleeding, 2010;53:3-11. A 68-year-old man presented with epigastric demonstrated increased vascular pattern (Figure 1B and pain for 2 weeks. The evidence base for endoscopic resection of duodenal adenomas is Discussion: limited, but it provides a promising result. They often have with the chance for complete removal ranges from 79 1-4 1-4 been discovered incidentally and usually asymptomatic. Duodenal adenomas have malignant potential in a similar fashion to colonic adenomas. Endoscopic management of with non-ampullary adenoma, and increases with the nonampullary duodenal polyps. Sporadic duodenal polyps: lower risk for malignant transformation than that of classification, investigation, and management. Because the morphological Prospective study of prevalence and endoscopic features plus their tendency to grow along folds, and histopathologic characteristics of duodenal duodenal adenomas can be more difficult to detect polyps in patients submitted to upper endoscopy. An 83-year-old man presented with epigastric Therefore, Nasogastroscopy with duodenal dilation was pain and melena. He has been taking aspirin for 8 performed successfully by a wire-guided balloon dilator. Figure 1: Duodenal stricture Figure 2: Post dilation of duodenal stricture Diagnosis: duodenal segments. The common site is duodenum Duodenal stricture pylorus and both duodenum and pylorus. The stricture pattern is usually either a short segment (2-3 mm in Discussion: length) or web-like circumferential narrowing. A 68-year-old man presented with maroon stool was then carried out but failed to identify the cause of for 2 days. One third of obscure gastrointestinal the treatment of bleeding gastrointestinal bleeding causes have been related to small bowel angiodysplasia-a retrospective evaluation. Long-term lesions were thought to arise from a degenerative outcome of patients treated with double balloon process associated with aging, local vascular anomalies, enteroscopy for small bowel vascular lesions. A 37-year-old woman presented with diarrhea, wall of the small bowel with multiple aortocaval, para abdominal pain and significant weight loss. Laboratory biopsy revealed diffuse infiltration with medium to results revealed severe hypoalbuminemia without large atypical lymphoid cells, of which, they were evidence of significant proteinuria. Discussion: Lymphoma is one of the most common References gastrointestinal malignancies and frequently involves 1. Gastrointestinal ileum is classically the most common site of small manifestations of malignant lymphoma. A 5 0 y e a r o l d w o m a n p r e s e n t e d w i t h the ongoing bleeding per rectum. She had been well until 3 deep ulcers with blood oozing it the distal jejunum weeks prior to admission; she had a low grade fever with and upper ileum (Figure 1-2). Finally, a 5 mg per kg of infliximab was colonoscopy revealed normal endoscopic appearance of infused intravenously, and the bleeding stopped the terminal ileum (Figure 3-4). Induction with the combination of Figure 3-4: Two months follow-up ileo-colonoscopy showed normal mucosa in terminal ileum Diagnosis: kg to control severe bleeding. Six of them stopped Severe small bowel bleeding in Crohn’s disease bleeding in one day after infliximab was infused. Endoscopic treatment, surgery and arterial embolization have been References used to control the massive gastrointestinal hemorrhage, 1. Inflixmab as a however, the management for severe gastrointestinal possible treatment for the hemorrhagic type of bleeding remains a great challenge. Acute hemorrhagic Crohn’s cause of bleeding, achieving mucosal healing is the disease controlled with infliximab. Crohn’s disease were prescribed with infliximab 5 mg per Case 12 Kittiyod Poovorawan, M. Biopsy form the ulcers confirmed the presence of carried out but the capsule failed to pass the pylorus jejunal metastasis of cholangiocarcinoma. Mid-gastrointestinal bleeding: capsule endoscopy and push-and-pull enteroscopy give Discussion: rise to a new medical term. Small intestinal bleeding can develop detectability, positive findings, total enteroscopy, from various causes such as vascular abnormality, ulcers, and complications of diagnostic double-balloon 2 diverticulum, and neoplasm. Previous reports of jejunal endoscopy: a systematic review of data over the metastasis were mostly from lung cancer and malignant first decade of use. Small intestinal metastasis from intrahepatic cholangiocarcinoma: report of a case. Her weight and symptom image revealed that the angle between superior gradually improved after jejunal feeding. Narrowing of duodenal portion between aorta and superior mesenteric artery (thick arrow) with mark dilatation of proximal duodenum and stomach (thin arrow), B. A B Figure 2: Direct endoscopic percutaneous jejunostomy: A) Needle punctured through proximal jejunum after illumination guidance, B) A snare was applied over the needle maintain the needle position. A B Figure 4: Endoscopic findings: A) the snare was switch to capture the catheter sheath and thread, B) A tread was pulled out and jejunostomy tube was placed by the pull technique. Leakage, plugging, tube fracture, migration and knotting are possible Discussion: 2 complications. Superior mesenteric artery syndrome is characterized by compression of the third portion of References duodenum due to narrowing space between the 1. The main component malfunction of percutaneous endoscopic of therapy is nutritional support. Enteral feeding distal to jejunostomy feeding tubes in patients with the obstruction such as jejunal tube or jejunostomy is intestinal dysmotility. A healthy 55-year-old man presented with month without any visible gastrointestinal bleeding. The chronic watery diarrhea with significant weight loss for a follow-up colonoscopy revealed worsening changes of year. There was no Therefore, double balloon enteroscopy was performed granuloma seen from the biopsy. Subsequently, exudate and inflamed surrounding mucosa along his hemoglobin dropped from 13 g/dl to 9 g/dl in a jejunum and ileum (Figure 1-6). J Gastroenteral (ileocolonoscopy and radiographic imaging) have been 2009;44:271-6. Diagnostic the yield is highest when the indication is to detect and therapeutic impact of double-balloon 2, 4, 5 stricture. A 73-year-old woman presented with maroon ulcer with a large non-bleeding visible vessel at proximal stool. One month high risk for vascular insufficiency from her underlying earlier, she was admitted at the intensive care unit due disease, antegrade embolization with Histoacryl injection to severe pneumonia with respiratory failure. Figure 1-2: A deep oval ulcer with a large non-bleeding visible vessel Figure 3: Histoacryl was injected directly into Figure 4: After histoacryl injection, mucosa was the visible vessel discolored Diagnosis: bipolar coaptation, hemoclipping, and argon plasma Small bowel ulcer with non-bleeding visible 3 coagulation. Bleeding are vascular ectasia, tumors, ulcerative diseases, and Dieulafoy lesions of the small bowel: a systematic 2 Meckel’s diverticula. Gastrointest Endosc 2011; endoscopic techniques in small bowel bleeding are 74:573-80. Microscopic examination showed Brunner gastric metaplasia with Helicobacter pylori. Figure 1: A duodenal polyp with erosion on top at duodenal bulb, size 6 mm in diameter (yellow arrow). Figure 2-4: A duodenal polyp with erosion on top at duodenal bulb, size 6 mm in diameter (yellow arrow). Figure 5-6: Microscopic examination showed a large polyp and containing structure was compatible with Brunner gland hyperplasia Diagnosis: Brunner glands, glandular lobulation and intervening Brunner gland hyperplasia 3 bands of paucicellular fibrous tissue. Endoscopic polypectomy is Brunner gland hyperplasia is not common considered for large, solitary, or suspected lesions to finding in duodenal bulb. The etiology and pathogenesis aid definitive diagnosis and prevent complications of these polyps are uncertain. Order lamisil with visa. Drink This After Fasting: Turmeric Golden Milk Shake: Thomas DeLauer.
Syndromes
|